Generic vs Brand Medications: What Really Matters for Your Health and Wallet
When you pick up a prescription, you might see two options: a generic medication, a drug that contains the same active ingredient as a brand-name version but is sold under its chemical name. Also known as generic equivalents, it is often significantly cheaper and approved by the same regulatory agencies as the original. And then there’s the brand name drug, the original version developed and marketed by a pharmaceutical company under a patent-protected name. Also known as originator drug, it usually costs more because the company recouped research and marketing expenses. The big question isn’t whether they’re different—it’s whether that difference actually affects you.
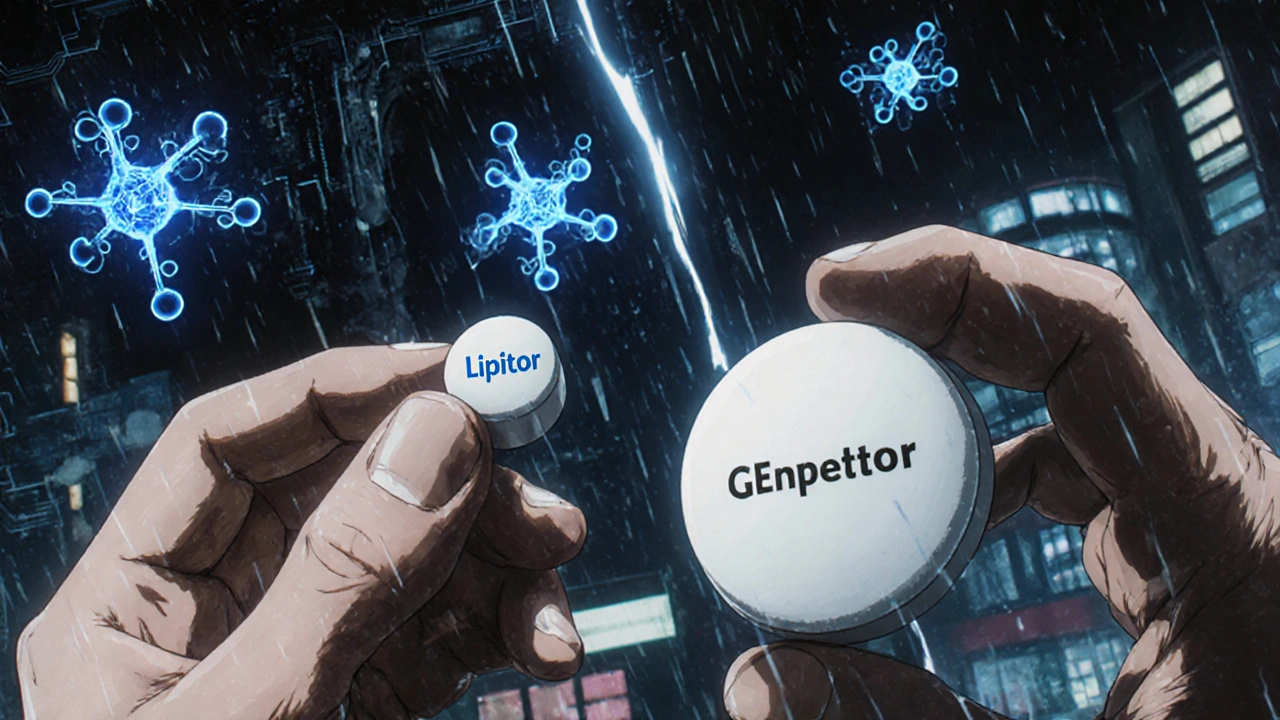
Here’s the truth: generic vs brand isn’t about quality. Both must meet the same strict standards for purity, strength, and how well they work in your body. The FDA requires generics to deliver the same amount of active ingredient at the same rate as the brand. That means if your doctor prescribes lisinopril, the generic version will lower your blood pressure just like Zestril. The fillers, color, and shape might change—that’s it. But here’s what does change: your wallet. A 30-day supply of brand-name Lipitor might cost $300. The generic atorvastatin? Often under $10. That’s not a trick. That’s the system working as intended.
Some people worry about switching. Maybe you’ve been on a brand for years and fear a change will mess with your body. But thousands of patients switch every day without issue. If you’ve had side effects, it’s rarely because the generic is inferior—it’s because your body reacts to inactive ingredients, like dyes or fillers. Talk to your pharmacist. They can check if your generic uses a different binder or coating that might trigger sensitivity. And if you’re on a drug with a narrow therapeutic window—like warfarin or levothyroxine—you should monitor closely after switching, but not because generics are less reliable. It’s because tiny changes in dose matter more in those cases.
Then there’s the legal side. generic patent law, the set of rules that govern when a brand-name drug can be copied by competitors. Also known as Hatch-Waxman Act, it created the whole system that lets generics enter the market after patents expire. Landmark court cases like Amgen v. Sanofi shape how long companies can delay generics. These legal battles don’t affect your daily pill—but they do affect how fast you get affordable options. That’s why some drugs stay expensive for years even after patent expiration.
And don’t forget the rise of digital pharmacies. They’re making it easier than ever to compare prices and order generics straight to your door. But that convenience comes with risks. Not all online sellers are legit. Always check if the pharmacy requires a prescription and is licensed in your state. A cheap generic from an unverified site could be fake, expired, or contaminated. Your health isn’t worth the gamble.
So what should you do? Ask your doctor if a generic is right for you. Ask your pharmacist if your current generic has changed manufacturers—sometimes the same drug from a new supplier causes unexpected reactions. And if cost is the issue, never skip your meds because you can’t afford them. There’s almost always a generic alternative. The system is designed to help you. You just need to know how to use it.
Below, you’ll find real-world comparisons, legal insights, and practical guides on switching from brand to generic—covering everything from blood pressure pills to antidepressants. No fluff. Just what works, what doesn’t, and what you need to know before your next refill.