Why Do So Many People Doubt Generic Drugs?
Imagine you’re at the pharmacy, holding two pills. One says Advil. The other says ibuprofen. They look different. One costs $5. The other costs $1. You’ve heard rumors. You wonder: is the cheaper one really the same? You’re not alone. Nearly 4 in 10 Americans still believe generic drugs are weaker, less safe, or not as effective as brand-name versions. That’s not just misinformation-it’s costing people money and health.
The truth? Generic drugs are required by the FDA to work exactly like their brand-name counterparts. They have the same active ingredient, the same strength, the same way they’re taken (pill, liquid, injection), and the same effect on your body. The only differences? Color, shape, and inactive fillers like starch or lactose-things that don’t affect how the drug works. But if you don’t know that, you’ll keep paying more than you need to.
What Exactly Makes a Drug “Generic”?
A generic drug isn’t a copy. It’s a legal, scientifically proven duplicate. The FDA demands that every generic drug delivers between 80% and 125% of the active ingredient in the bloodstream compared to the brand-name version. That’s not a guess. It’s based on real blood tests done in hundreds of volunteers. If a generic doesn’t meet that standard, it doesn’t get approved.
Take atorvastatin, the generic version of Lipitor. A 2016 study of over 8,600 heart patients found no difference in cholesterol control or heart attack risk between the two. Same drug. Same results. Same safety profile. Yet many patients still refuse the generic because they think it’s “less medicine.”
Even more surprising? The FDA requires generics to be made in the same kind of facilities as brand-name drugs. Many brand-name companies actually make their own generics under different labels. These are called authorized generics. They’re identical to the brand-same factory, same formula, same packaging-just without the fancy name and price tag. They’ve been shown to have 28% fewer patients switching back to the brand, because people trust them more.
How Do Language Guides Help Patients Understand?
Most drug information is written for doctors-not patients. A typical FDA document reads like a college textbook. Readability score? 14.2. That means you’d need a college education to understand it. But most patients don’t have that. That’s where consumer language guides come in.
These guides use simple words, short sentences, and real-life comparisons. Instead of saying “bioequivalence,” they say: “It’s like buying store-brand cereal instead of Kellogg’s. Same ingredients, same nutrition, half the price.”
Pharmacies like CVS, Walgreens, and Walmart now train their staff to explain generics in 90 seconds using three clear points:
- Same active ingredient-the part that actually works (e.g., 20mg esomeprazole in both Nexium and its generic).
- Same effect-it works the same way in your body, within FDA-approved limits.
- Same savings-on average, $387 per prescription per year.
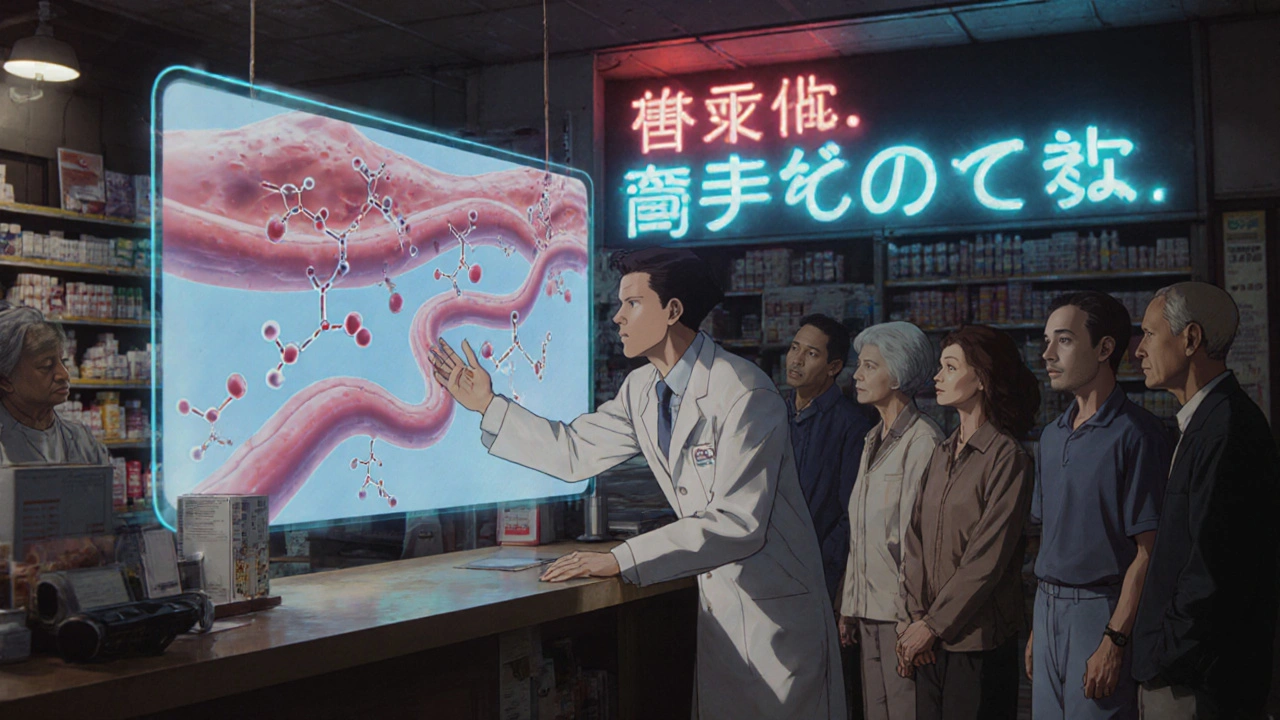
They also use visual aids. Side-by-side photos of brand and generic pills. Charts showing how the same chemical name-N-(4-hydroxyphenyl) acetamide-is also called acetaminophen and sold as Tylenol. This simple “What’s In a Name?” chart from the FDA has cut patient confusion by 82%, according to pharmacists who use it.
When Are Generics Not Exactly the Same?
Most of the time, generics are perfect replacements. But there are exceptions. For drugs with a narrow therapeutic index, even tiny changes in how the body absorbs the medicine can matter. These include:
- Levothyroxine (for thyroid issues): Some patients report feeling worse after switching. Studies show inconsistent absorption between brands and generics. The American Association of Clinical Endocrinologists recommends sticking with the same maker once you find one that works.
- Warfarin (a blood thinner): Small differences in absorption can lead to dangerous bleeding or clots. Many doctors still prefer the brand for this one.
- Phenytoin (for seizures): A 2010 study found certain generics led to 17% more breakthrough seizures in some patients.
That’s why the best language guides don’t say “all generics are identical.” They say: “Most generics are just as good. But for some medicines, your doctor might recommend sticking with one brand.”
And if you’re on one of these drugs? Don’t switch without talking to your doctor. Keep using the same generic maker. If you notice changes-fatigue, dizziness, mood swings-tell your provider. It’s not in your head. It’s real.
Why Do People Still Avoid Generics?
It’s not just about money. It’s about fear. People worry:
- “Is this fake?”
- “Did they cut corners?”
- “Will it make me sicker?”
These fears come from bad experiences. In 2012, the FDA pulled a generic version of Wellbutrin XL because it didn’t release the drug properly. That was one bad batch. But it made headlines. And now, people remember it.
Another issue? Oversimplification. Some guides say, “Generics are exactly the same.” That’s true for most drugs. But not all. When patients later learn there are exceptions, they feel misled. Trust breaks down.
Good language guides fix this. They say: “For most medicines, yes. For a few, maybe not. Here’s how to know.” They don’t pretend everything is black and white. They give the full picture-clearly, honestly, simply.

What’s New in 2025?
Things are changing fast. In January 2025, all Medicare Part D plans must give patients generic education materials that meet NIH health literacy standards. That means no more confusing brochures. No more 10-page PDFs. Just clear, simple, visual guides you can read in under five minutes.
Pharmacies are also testing AI tools that personalize the explanation. If you have low health literacy, the system gives you simpler words. If you’re on a high-risk drug like levothyroxine, it highlights the warning. If you’ve had trouble with generics before, it suggests staying with your current brand.
And the FDA? They’ve launched a $4.7 million program to build medication-specific guides for the 20 most common narrow therapeutic index drugs. These aren’t generic advice. They’re targeted advice for your exact medicine.
What You Can Do Today
You don’t need to wait for a new guide. Here’s how to get the right info now:
- Ask your pharmacist: “Is this generic the same as the brand? Are there any risks for my medicine?”
- Check the FDA’s website: Go to fda.gov/genericdrugs. They have updated charts, videos, and FAQs updated quarterly.
- Use the “teach-back” trick: After they explain, say: “So, to make sure I got it right-you’re saying this generic works the same as the brand because…” If you can explain it back, you understand it.
- Stick with one maker for drugs like levothyroxine or warfarin. Don’t switch brands unless your doctor says it’s safe.
- Look for authorized generics: These are brand-name drugs sold under a generic label. They’re the closest thing to the original. Ask your pharmacist: “Is there an authorized generic for this?”
Final Thought: You’re Not Being Scammed
Generic drugs saved the U.S. healthcare system nearly $2 trillion between 2009 and 2019. That’s money that went back into hospitals, doctors’ offices, and patients’ pockets. But none of that matters if people won’t use them.
The problem isn’t the drugs. It’s the message. When we stop talking like pharmacists and start talking like neighbors-with honesty, clarity, and real examples-we win. We save money. We get better care. We trust the system again.
Next time you’re handed a cheaper pill, don’t hesitate. Ask. Learn. Understand. And remember: your health doesn’t care what’s printed on the label. It only cares if the medicine works.
Are generic drugs really as effective as brand-name drugs?
Yes, for the vast majority of drugs. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also deliver the same amount of medicine into your bloodstream-within a tight range of 80% to 125%. This is proven through clinical testing. Studies show that for drugs like atorvastatin, metformin, and sertraline, generics work just as well as brands. The only exceptions are a small number of drugs with narrow therapeutic indexes, like levothyroxine or warfarin, where even small differences in absorption can matter.
Why do generic pills look different from brand-name pills?
By law, generic drugs can’t look exactly like the brand-name version, so they’re made in different colors, shapes, or sizes. But that’s only because of trademark rules-not because of effectiveness. The differences are in inactive ingredients like dyes, fillers, or coatings. These don’t affect how the drug works. For example, one brand of ibuprofen might be white and oval, while the generic is blue and round. But both contain the same 200mg of ibuprofen and work the same way in your body.
Can I switch between different generic brands?
For most medications, yes. But for drugs like levothyroxine, warfarin, or phenytoin, it’s better to stick with the same manufacturer. Even though all generics meet FDA standards, slight differences in how the drug is absorbed can affect how you feel. If you switch and notice new symptoms-like fatigue, dizziness, or mood changes-tell your doctor. Many people do better when they use the same generic version consistently.
What’s an authorized generic?
An authorized generic is the exact same drug as the brand-name version, but sold without the brand name and at a lower price. It’s made by the same company, in the same factory, with the same ingredients and packaging. The only difference? It doesn’t carry the brand logo. These have been shown to have 28% fewer patients switching back to the brand because they’re trusted more. Ask your pharmacist: “Is there an authorized generic for this medicine?”
Why do some doctors still prescribe brand-name drugs?
For most patients, generics are the right choice. But for a few high-risk drugs-like levothyroxine, warfarin, or certain seizure medications-some doctors prefer to stick with a brand they’ve seen work consistently over time. This isn’t about distrust in generics. It’s about minimizing risk in situations where small changes in drug levels could cause serious problems. If your doctor recommends a brand, ask why. They may be following a guideline for your specific condition.

Andrea Johnston
November 18, 2025 AT 21:14My pharmacist showed me the FDA chart. Same active ingredient. Same chemistry. Just no fancy logo. It’s not magic-it’s science.
Scott Macfadyen
November 20, 2025 AT 18:33Chloe Sevigny
November 21, 2025 AT 07:30Denise Cauchon
November 21, 2025 AT 12:13Here, generics are the default. No one bats an eye. We don’t pay $100 for a pill that’s been proven to work the same. Stop being manipulated by Big Pharma ads. Your body doesn’t care about the logo.
Victoria Malloy
November 21, 2025 AT 22:15Gizela Cardoso
November 23, 2025 AT 04:27Alex Czartoryski
November 24, 2025 AT 18:05Angela J
November 26, 2025 AT 04:59Sameer Tawde
November 27, 2025 AT 12:32Saket Sharma
November 29, 2025 AT 05:07Shravan Jain
November 30, 2025 AT 09:42Brandon Lowi
November 30, 2025 AT 20:05Joshua Casella
December 2, 2025 AT 02:03Alex Boozan
December 3, 2025 AT 21:42mithun mohanta
December 5, 2025 AT 10:22