When you pick up a prescription, you might see two options on the receipt: the brand-name version and a cheaper generic. It’s easy to assume the brand is better. But here’s the truth: generic drugs work the same way, cost far less, and are held to the exact same safety standards. The real difference isn’t in effectiveness-it’s in the price tag.
What exactly is a generic drug?
A generic drug is the exact same medicine as the brand-name version, just without the marketing. It contains the same active ingredient, in the same strength, and works the same way in your body. The FDA requires generics to be bioequivalent-meaning they deliver the same amount of medicine into your bloodstream at the same rate as the brand. That’s not a guess. It’s a strict rule. The acceptable range? Within 80% to 125% of the brand’s performance. In real terms, that means your body absorbs it just like the original.
Generic drugs aren’t copies or imitations. They’re identical in function. The only differences are in the inactive ingredients-like fillers, dyes, or flavorings-which don’t affect how the drug works. That’s why a generic ibuprofen tablet might look different from Advil, but it reduces your headache just as fast.
Why are generic drugs so much cheaper?
Brand-name drugs cost a lot because the company that invented them had to pay for years of research, clinical trials, and marketing. Those costs get baked into the price. Once the patent expires-usually after 10 to 12 years-other companies can make the same drug. They don’t need to repeat expensive tests. Instead, they file a simpler application called an ANDA (Abbreviated New Drug Application) and prove bioequivalence. That cuts their costs dramatically.
As soon as the first generic enters the market, prices start dropping. With one competitor, the price falls to about 90% of the brand’s cost. With three or four generics, it drops to 60-70%. And when five or more companies start making it? The price often falls below 50% of the original. The FDA estimates that generics cost 79% to 85% less than brand-name drugs. That’s not a rumor. It’s backed by data from the Association for Accessible Medicines, which found that in 2024, generics made up 90% of all prescriptions filled in the U.S.-but only 12% of total drug spending.
Brand-name drugs are getting cheaper too
Here’s something most people don’t realize: brand-name drug prices are falling in many cases-not because of generosity, but because of competition. When a generic is about to launch, manufacturers sometimes lower their own prices to stay competitive. In 2025, Bayer cut the list price of Nexavar by 50% after its first generic version hit the market. Merck reduced Januvia and related drugs by 42.4%. These aren’t isolated moves. DrugChannels found that brand-name drug prices have been declining for seven straight years.
Why? Because the financial pressure is real. Medicare and private insurers are pushing back. The Inflation Reduction Act will force Medicare to negotiate prices on certain high-cost drugs starting in 2026. Companies know they can’t keep charging $10,000 a month for a drug when a generic version costs $10. So they’re adjusting-sometimes before the generic even arrives.
But list price isn’t the whole story
There’s a big gap between what a drug is listed at and what’s actually paid. That’s called the gross-to-net gap. Brand-name manufacturers often offer huge discounts and rebates to pharmacies and insurers. In 2024, while list prices rose slightly, net prices (what insurers actually pay) barely moved. The gap was just -2.2%, meaning manufacturers gave back almost everything they gained in list price hikes.
Generics don’t play this game. There are no rebates, no complex negotiations. The price you see at the pharmacy is usually the price you pay. That’s why generics are so predictable-and why they’re the only part of the drug market where spending has actually gone down. Since 2019, total spending on generics has dropped by $6.4 billion, even though more people are using them. That’s because prices keep falling as more companies enter the market.
Are generics really as safe and effective?
Yes. The FDA requires generics to meet the same strict standards as brand-name drugs for quality, strength, purity, and stability. They’re made in the same type of facilities, under the same rules. The American Medical Association and the FDA both say generics are interchangeable with brands when appropriate.
Still, 62% of Americans say they trust brand-name drugs more. Why? Mostly because of branding. You’ve seen the ads. You know the logo. You’ve heard the name for years. But trust isn’t the same as science. A 2025 Tebra survey found that 84% of Americans believe generics are just as effective. And 63% choose them because they’re cheaper-not because they’re unsure of the brand.
There are rare exceptions. For drugs with a narrow therapeutic index-like warfarin, levothyroxine, or some epilepsy meds-doctors sometimes prefer to stick with one version to avoid tiny variations in absorption. But even then, switching between generics is usually fine. The key is consistency: if you start on a generic, stay on it. Don’t switch back and forth unless your doctor says to.
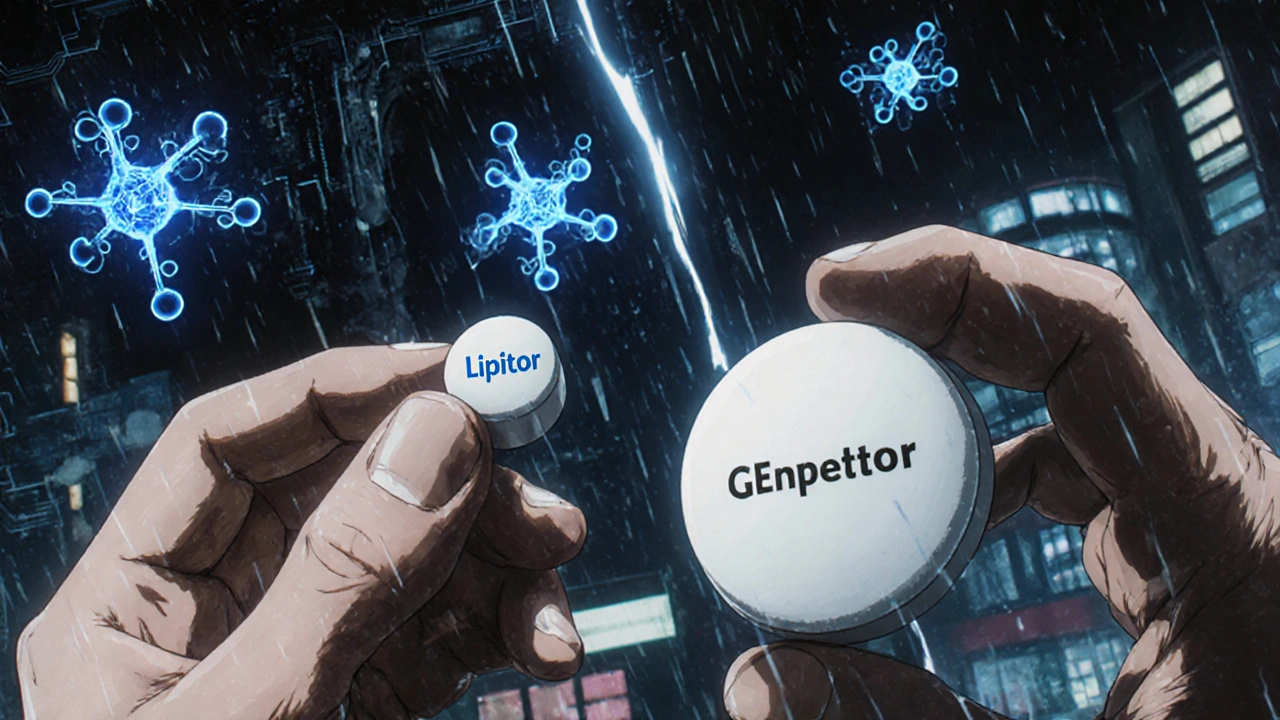
How much can you really save?
Let’s look at real numbers. A 30-day supply of the brand-name drug Lipitor (atorvastatin) might cost $150 without insurance. The generic version? Around $10. That’s a 93% savings.
For metformin (a common diabetes drug), the brand Glucophage costs about $120. The generic? $4. That’s a 97% drop.
Even for expensive specialty drugs, the savings are massive. The brand-name drug Revcovi costs around $200,000 per prescription. There’s no generic yet, so the price stays high. But when a generic does come out, history shows the price will collapse-likely to under $10,000. That’s the power of competition.
Here’s a quick look at typical savings based on how many generic makers are in the market:
| Number of Generic Manufacturers | Price Relative to Brand |
|---|---|
| 1 | ~90% of brand price |
| 3-4 | 60-70% of brand price |
| 5+ | Below 50% of brand price |
What about biosimilars?
Biosimilars are the generic version of biologic drugs-complex medicines made from living cells, like Humira or Enbrel. They’re not exact copies like small-molecule generics, but they’re proven to work the same way. The FDA requires them to show no meaningful difference in safety or effectiveness. Biosimilars cost 15-35% less than their brand-name counterparts, and that gap is growing as more enter the market. They’re the future of lowering costs for cancer, autoimmune, and chronic disease treatments.
When should you choose a brand over a generic?
Almost never. Unless your doctor has a specific medical reason-not just preference-you should take the generic. The only times you might consider the brand are:
- You had a bad reaction to a specific generic filler (very rare)
- You’re on a drug with a narrow therapeutic index and your doctor wants you to stay on one version
- Your insurance doesn’t cover the generic (uncommon)
Even then, ask your doctor: Is this really necessary? Or is it habit? Most of the time, the answer is: no.
How to get the best deal on prescriptions
Even if you’re taking a generic, you can still save more:
- Use pharmacy discount apps like GoodRx or SingleCare-often they beat your insurance price
- Ask for a 90-day supply instead of 30-many generics are cheaper per pill in bulk
- Check if your pharmacy has a $4 generic list (many do for common meds like metformin, lisinopril, or atorvastatin)
- Don’t assume your insurance will automatically pick the cheapest option-ask them to switch you to the generic if you’re on the brand
And remember: if you’re on Medicare, the new $2,000 out-of-pocket cap in 2025 will make generics even more valuable. The lower your drug costs, the faster you hit that cap-and the less you pay after that.
Why does this matter beyond your wallet?
Generic drugs don’t just save you money-they keep the whole system working. Without generics, prescription spending in the U.S. would be nearly triple what it is now. That’s not theoretical. The University of Chicago’s 2025 study found that the U.S. has lower overall prescription costs than peer countries like Canada, Germany, and the UK-not because brand drugs are cheap, but because generics are dirt cheap.
That’s the secret: high-priced brand drugs fund innovation. Low-priced generics make treatment accessible. The system works because both exist. And you benefit from both.
Choosing a generic isn’t settling. It’s smart. It’s science-backed. And it’s how millions of Americans afford their meds every day.
Are generic drugs really as good as brand-name drugs?
Yes. Generic drugs contain the same active ingredient, in the same strength and dosage form, and work the same way in your body. The FDA requires them to meet the same strict standards for quality, safety, and effectiveness as brand-name drugs. The only differences are in inactive ingredients like color or filler, which don’t affect how the drug works.
Why do generics cost so much less?
Brand-name drug companies spend billions on research, clinical trials, and marketing. Generics don’t have to repeat those expensive tests. Once a patent expires, other manufacturers can produce the drug by proving it’s bioequivalent to the original. This cuts their costs dramatically, allowing them to sell at 79-85% lower prices.
Can I trust generic drugs from different manufacturers?
Yes. All generic manufacturers must meet FDA standards, regardless of the company. The FDA inspects their facilities and reviews their production processes. Switching between different generic brands is safe and common. The only time you might want to stick with one is if you’re on a drug with a narrow therapeutic index and your doctor recommends consistency.
Why do some people still prefer brand-name drugs?
Many people trust brands because of advertising, familiarity, or past experiences. But this is perception, not science. A 2025 survey found that while 62% of Americans trust brand-name drugs more, 84% believe generics are just as effective. Most people choose generics because they’re cheaper-not because they doubt their quality.
Do generic drugs take longer to work?
No. Generic drugs must be bioequivalent to the brand, meaning they deliver the same amount of medicine into your bloodstream at the same speed. Any difference in how quickly you feel relief is likely due to placebo effect or unrelated factors like diet or stress-not the drug itself.
Is it safe to switch from a brand to a generic?
Yes, for most medications. The FDA approves these switches. But if you’re on a drug with a narrow therapeutic index-like warfarin, thyroid meds, or seizure drugs-talk to your doctor first. They may recommend staying on the same version to avoid tiny variations in absorption. Otherwise, switching is safe and common.
What if my insurance won’t cover the generic?
That’s rare, but if it happens, ask your pharmacist or insurance company why. Sometimes it’s a system error. You can also ask your doctor to request a prior authorization for the generic, or use a discount app like GoodRx to pay cash-often cheaper than your insurance copay.
Will generic drugs become even cheaper in the future?
Yes. As more companies enter the market after patent expirations, prices keep falling. The more competition, the lower the price. With over 90% of prescriptions now filled with generics, the trend is clear: affordability will keep improving. New biosimilars for expensive biologics are also entering the market, which will bring similar savings to complex treatments like cancer and autoimmune drugs.
Bottom line: if you’re taking a brand-name drug and a generic is available, ask your doctor or pharmacist about switching. You’ll get the same results for a fraction of the cost. That’s not a compromise-it’s common sense.
Noel Molina Mattinez
November 17, 2025 AT 13:39Generics work fine
Christina Abellar
November 18, 2025 AT 12:22Same active ingredient, same results. Why pay more?
Margo Utomo
November 20, 2025 AT 07:44Generics saved me $120/month on my blood pressure med 🙌 I used to think brand was better… until my wallet cried. Now I’m a convert. 💊✨
Georgia Green
November 22, 2025 AT 05:58i always use genercs but once i got one that made me feel weird like dizzy? turned out it was just the new filler, switched back and fine. not all generics are equal but most are perfect
Eva Vega
November 23, 2025 AT 22:50From a pharmacoeconomic standpoint, the bioequivalence threshold of 80–125% AUC and Cmax is well within the margin of clinical insignificance for the vast majority of pharmaceutical agents. The cost-savings paradigm is statistically and clinically validated by CMS and FDA datasets.
Dave Feland
November 24, 2025 AT 02:55Did you know the FDA allows generics to vary by up to 25% in absorption? That’s not science-that’s a loophole. Big Pharma and the FDA are in cahoots. I switched to imported meds from Canada. At least there, they test properly.
Ashley Unknown
November 25, 2025 AT 00:10Okay but have you ever heard of the Great Generic Switch of 2021? My cousin’s mom had a seizure after switching from brand to generic levothyroxine. The hospital bill was $87,000. The FDA knew about the absorption variance but didn’t warn anyone. They’re hiding it because drug companies pay them. And now they’re pushing biosimilars next-same playbook. I’m not taking any more pills until this is investigated. I’ve been researching this for 14 months. I have spreadsheets. I have emails. Someone needs to listen.
Sylvia Clarke
November 26, 2025 AT 06:57It’s funny how we trust a $200 brand pill more than a $10 generic-even though they’re chemically identical. We’ve been conditioned by ads, logos, and the illusion of prestige. The real luxury isn’t the brand name-it’s the peace of mind that comes from knowing you’re not being ripped off. I’ve been on generics for 12 years. My cholesterol’s perfect. My bank account’s happier. And I haven’t missed a beat.
Let’s be real: if your doctor pushes brand over generic without a medical reason, they’re either lazy or getting kickbacks. Not all, but enough. Ask for the generic. Always. Your future self will thank you.
And yes, I’ve switched between six different generic manufacturers of metformin. No side effects. No drama. Just lower copays and better sleep at night.
Why does this matter? Because 1 in 4 Americans skip doses because they can’t afford meds. Generics aren’t a compromise-they’re a lifeline. And if you’re still skeptical, try this: take your brand-name drug for a month, then switch to generic. Keep a journal. You’ll see zero difference. But you’ll save hundreds.
It’s not about trust. It’s about math. And math doesn’t lie.
Matt Wells
November 27, 2025 AT 21:24While the data presented is statistically sound, one must not overlook the regulatory capture inherent in the FDA’s ANDA approval process. The agency relies on industry-submitted bioequivalence data, which introduces a profound conflict of interest. Moreover, the 80–125% bioequivalence window, while technically permissible, is not physiologically inert for all patient subpopulations-particularly the elderly, renally impaired, or those on polypharmacy regimens.
The assertion that generics are universally interchangeable is a dangerous oversimplification. The FDA’s own post-market surveillance data reveals a 3.7% increase in adverse event reports following generic substitution for narrow-therapeutic-index drugs, even when manufacturers comply with regulatory thresholds.
Furthermore, the claim that brand-name prices are declining due to competition is misleading. The majority of price reductions are offset by increased rebates to PBMs, which are opaque and non-transparent to the consumer. The net price may be stable, but the gross-to-net gap continues to widen, enriching middlemen while the patient pays the same.
Therefore, while generics serve a valuable function, their universal endorsement without individualized clinical assessment is a form of pharmaceutical paternalism.
George Gaitara
November 28, 2025 AT 07:25Why are we even talking about this? Everyone knows generics are just as good. This article is just rehashing basic pharmacy 101. Do you really need a 2,000-word guide to tell people not to overpay? I mean… come on. The real story is how the system still lets people pay $150 for Lipitor when it’s been generic for a decade. That’s not about science-that’s about greed.
Roberta Colombin
November 29, 2025 AT 00:25Thank you for sharing this clear and important information. Many people are afraid to switch to generic medications because they do not understand how they are regulated. It is reassuring to know that the same strict standards apply. I have encouraged my elderly neighbors to ask their pharmacists about generics, and many have saved over $100 per month. This is a small change that makes a big difference in people’s lives.
Margo Utomo
November 30, 2025 AT 07:36PS: I just used GoodRx to get my generic lisinopril for $3. I’m basically getting free medicine now. 🤑💊 #GenericsAreMagic
Georgia Green
December 1, 2025 AT 11:15wait i just realized my doctor wrote me a brand name for my generic… i asked the pharmacist and they said they can switch it for free. i feel dumb. thanks for reminding me to ask