Periodic Limb Movement Disorder: Causes, Symptoms, and What You Can Do
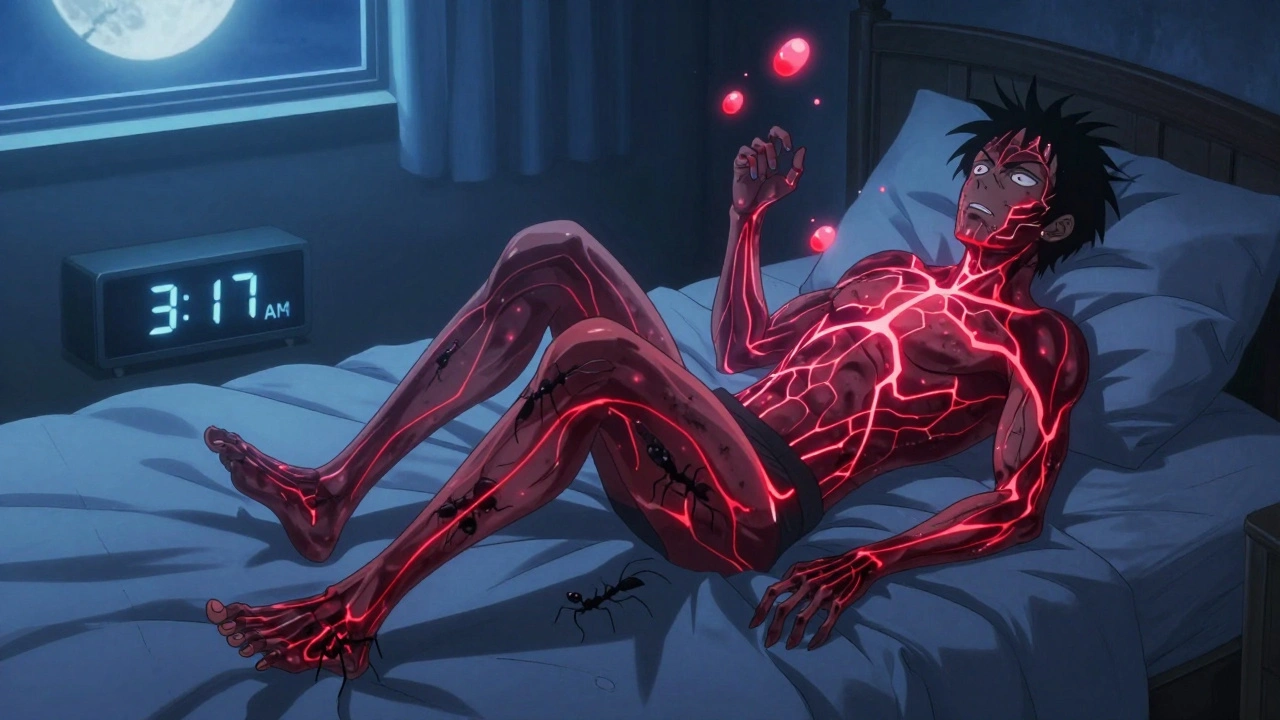
When you or your partner keep waking up because of sudden leg jerks during sleep, it might not just be restlessness—it could be periodic limb movement disorder, a sleep condition where limbs move involuntarily in rhythmic patterns, usually during non-REM sleep. It’s often confused with restless legs syndrome, but they’re not the same: one happens while awake and urges movement, the other happens while you’re asleep and you don’t feel it. Many people with this disorder don’t even know they have it until someone else notices the kicking or twitching. And if you’re constantly tired in the morning, even after 8 hours in bed, this could be why.
restless legs syndrome, a neurological condition causing uncomfortable sensations in the legs and an urge to move them, especially at night often shows up alongside periodic limb movement disorder. About 80% of people with restless legs also have limb movements during sleep. But you can have the movements without the urge—that’s the key difference. Iron levels, kidney disease, diabetes, and certain medications like antidepressants can make both worse. If you’re on a drug for depression or nausea, it might be worth asking your doctor if it’s contributing to your sleep disruptions.
It’s not just about tossing and turning. Left untreated, this disorder can lead to chronic insomnia, daytime fatigue, mood swings, and even high blood pressure over time. You won’t remember the movements, but your body does. And if you’re struggling with sleep quality, it’s not just "getting old"—it’s a medical issue that can be managed. Simple changes like cutting caffeine after noon, avoiding alcohol before bed, or checking your iron levels can make a big difference. In some cases, doctors prescribe medications that calm nerve signals, but those aren’t always needed.
What you’ll find in the posts below aren’t generic sleep tips. They’re real, evidence-based insights from people who’ve dealt with medication side effects, drug interactions, and how conditions like heart failure or diabetes can quietly wreck your sleep. You’ll see how anticoagulants, blood thinners like warfarin and DOACs that require careful management to avoid bleeding risks might affect sleep patterns, how statin intolerance, muscle pain from cholesterol drugs that can disrupt sleep and lead to stopping treatment is more common than you think, and how tinnitus, ringing in the ears that can make falling asleep nearly impossible often overlaps with movement disorders in older adults. These aren’t random articles—they’re connected. Because sleep doesn’t happen in a vacuum. It’s tied to your meds, your nerves, your heart, and your overall health.