Restless Legs Syndrome Isn’t Just Discomfort - It’s a Sleep Killer
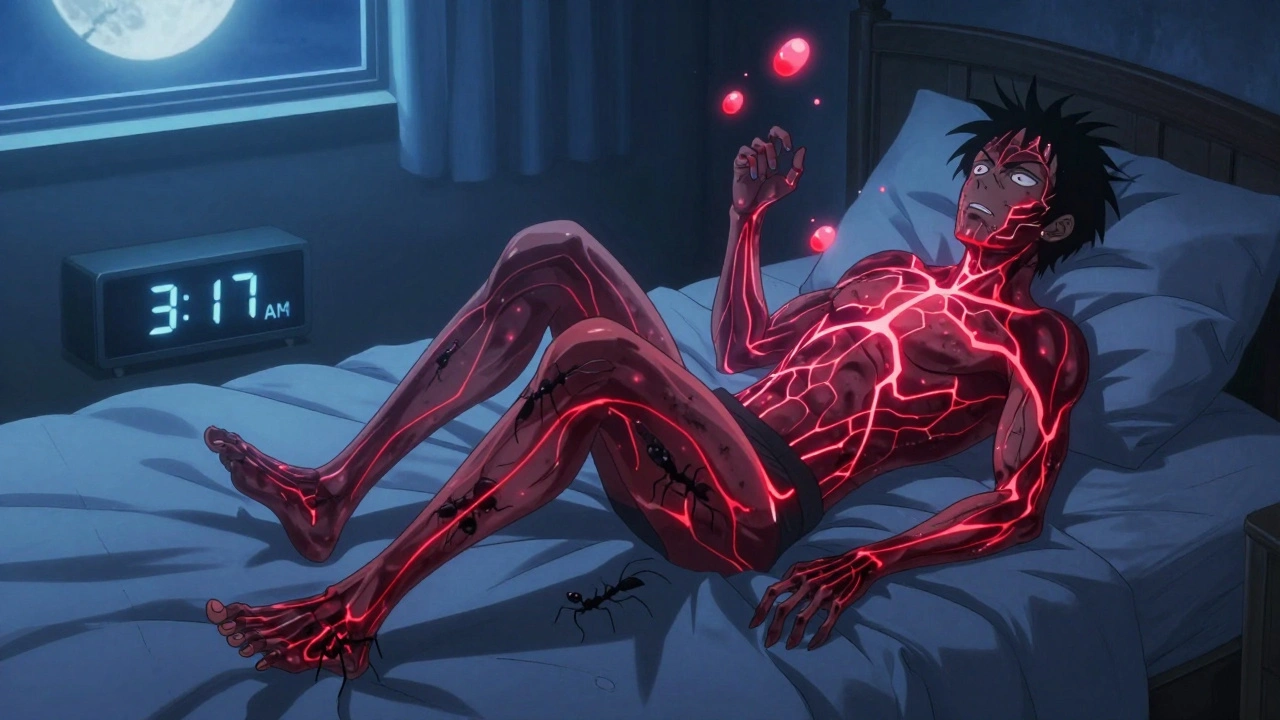
If you’ve ever lain awake at night, your legs twitching, crawling, or aching with an urge to move that no amount of stretching can fix, you’re not alone. About 1 in 10 adults in the U.S. live with Restless Legs Syndrome (RLS), also called Willis-Ekbom disease. For many, it’s not just an annoyance - it’s a thief of sleep, energy, and mental clarity. Symptoms don’t just show up at night; they hijack your entire life. You might feel fine during the day, but as soon as you sit down to relax or lie in bed, the sensations return - sharp, electric, or like ants crawling under your skin. The only relief? Moving. Standing up. Walking. Shaking your legs. But when you’re trying to sleep, that’s not an option.
Polysomnography studies show people with RLS lose 30-50% of their total sleep time. They spend more time in shallow, unrefreshing sleep (N1 and N2 stages) and less in deep, restorative sleep. On average, they take 45 to 60 minutes just to fall asleep - double the time of someone without RLS. And once asleep? They wake up 6 to 10 times a night, often without even realizing why. The result? Daytime exhaustion, brain fog, and a 2.3 times higher risk of car accidents. This isn’t insomnia. It’s a neurological disorder with a very specific biological cause.
Why Your Brain Is the Real Culprit
RLS isn’t caused by bad sleep habits, stress, or caffeine. It’s rooted in your brain’s dopamine system. Dopamine is the chemical that helps your brain control movement and regulate sensation. In RLS, something goes wrong with the A11 dopaminergic neurons - the ones that send signals from your brain down to your spinal cord. Brain scans show these patients have 20-30% less dopamine transporter activity in the striatum compared to healthy people. That means dopamine isn’t being recycled properly. The signal gets messy. And your legs? They interpret that as pain, tingling, or an unbearable need to move.
Iron plays a big role too. Low iron levels in the substantia nigra - the same brain region affected in Parkinson’s - are found in up to 70% of RLS patients. Iron is needed to make dopamine. No iron? Less dopamine. That’s why checking serum ferritin levels is now standard practice. If your ferritin is below 75 ng/mL, iron therapy (often via IV infusion) can cut symptoms by 30-40%. But it takes months to work. And for many, that’s too slow.
Most people with RLS also have Periodic Limb Movement Disorder (PLMD). That’s when your legs jerk every 20-40 seconds during sleep - sometimes 15 to 100 times an hour. These movements don’t wake you up directly, but they fragment your sleep cycles. You don’t remember them. But your body does. And that’s why you wake up tired, even after 8 hours in bed.
Dopaminergic Therapy: Fast Relief, High Risk
For years, the go-to treatment for moderate to severe RLS has been dopamine-boosting drugs. Three are FDA-approved: ropinirole (Requip), pramipexole (Mirapex), and rotigotine (Neupro). They work fast - usually within an hour. Patients report being able to finally sleep through the night after years of suffering. That’s why these drugs are still the first choice for many doctors.
But here’s the catch: they don’t fix the problem. They mask it. And over time, they make it worse.
Augmentation is the biggest problem. That’s when RLS symptoms start earlier in the day - maybe even at noon - spread to your arms or torso, and become more intense. In clinical trials, 20-70% of patients develop augmentation within a year. Pramipexole has the highest rate - up to 66% after three years. Rotigotine, the patch, is better, at just 26%. The reason? Dopamine agonists overstimulate receptors. Your brain gets used to the boost. Then it starts demanding more. You increase the dose. The symptoms get worse. You’re trapped in a cycle.
Another hidden danger? Impulse control disorders. About 6-17% of patients develop compulsive behaviors - gambling, shopping, binge eating, even hypersexuality. One patient reported $20,000 in credit card debt from uncontrollable online shopping. Men with prior mental health issues are at higher risk. The FDA added black box warnings to all dopamine agonists in 2016. That means doctors are legally required to warn patients. But many don’t. Or patients don’t connect the dots.
What Works Better in the Long Run?
There’s a better option: alpha-2-delta ligands. These include gabapentin enacarbil (Horizant), pregabalin (Lyrica), and gabapentin. They don’t touch dopamine. Instead, they calm overactive nerves. They take longer - 2 to 4 weeks to kick in - but they don’t cause augmentation. In a major 2021 trial, pregabalin worked just as well as pramipexole at reducing symptoms, but with only 8% augmentation versus 32%.
And here’s something most people don’t know: iron therapy isn’t just for the severely deficient. Even mild iron deficiency (ferritin 30-75 ng/mL) can make RLS worse. Oral iron is often too slow. IV ferric carboxymaltose works faster. One study showed symptom improvement in 80% of patients after three infusions. It’s not a cure. But it’s a foundation. And it’s safe.
Non-drug approaches matter too. Regular moderate exercise - like walking or cycling - helps. Avoiding alcohol, caffeine, and nicotine after 2 p.m. reduces flare-ups. Some patients swear by leg massages, warm baths, or compression socks. They won’t fix the root cause, but they can make nights more bearable.
The Real Cost - Not Just Money, But Quality of Life
RLS isn’t cheap. In the U.S., annual direct medical costs average $2,800 to $4,200 per patient. Dopamine agonists cost $800-$1,200 a year. Alpha-2-delta ligands? $1,500-$2,000. But the hidden cost is worse. Lost productivity. Missed family time. Depression. Anxiety. A 2022 meta-analysis found RLS patients had 20-30% lower scores on attention and memory tests. That’s not just tiredness - it’s brain function impaired by chronic sleep loss.
Market data shows dopamine agonists still make up 55% of the $1.2 billion RLS treatment market. But growth is slowing. Rotigotine is rising because it causes less augmentation. And new drugs are coming. A new extended-release form of ropinirole (Requip XL) cut augmentation rates from 31% to 18% in 12 months. Fipamezole, an alpha-2 adrenergic antagonist, is in Phase II trials and looks promising. Intranasal apomorphine could offer fast relief without long-term exposure.
But the biggest shift is in thinking. The International Restless Legs Syndrome Study Group now recommends alpha-2-delta ligands as first-line for chronic RLS. Dopamine agonists? Reserved for intermittent symptoms or severe cases that don’t respond to anything else.

What You Need to Do - A Realistic Roadmap
If you think you have RLS, don’t just assume it’s “just nerves.” Get tested. Start with a blood test for ferritin. If it’s below 75 ng/mL, talk to your doctor about IV iron. Don’t wait months for oral supplements to work.
Keep a symptom diary. Note when symptoms start, how bad they are (on a scale of 0-10), and whether they spread. This is the best way to catch augmentation early. A 2022 study found 83% of cases were spotted within three months using this method.
Don’t start dopamine agonists unless you have to. If you’re on them, ask: Is this still working? Are symptoms starting earlier? Are you feeling urges to gamble, shop, or eat compulsively? If yes, talk to your doctor. Don’t wait for it to get worse.
For long-term management, alpha-2-delta ligands are safer. They’re not perfect - they can cause dizziness or weight gain - but they don’t rewire your brain like dopamine drugs do. And they work.
RLS isn’t curable. But it’s manageable. And the key isn’t just medication. It’s understanding your brain, your iron, and your sleep. The best outcomes come from combining iron therapy, non-dopamine meds, and lifestyle tweaks. Not just a pill at bedtime.
What Comes Next
Researchers are now looking at genetics. Variants in the BTBD9 and MEIS1 genes are linked to RLS risk and treatment response. A 2022 study showed a 72% accuracy rate in predicting who will respond to pramipexole based on genetic profile. That’s the future: personalized treatment. No more trial and error.
For now, the message is clear: dopamine agonists work - fast. But they’re not a long-term solution. They’re a bridge, not a destination. The real win? Getting your iron up, switching to safer meds, and reclaiming your nights - without trading one problem for another.
Sandridge Nelia
December 3, 2025 AT 23:09Mark Gallagher
December 4, 2025 AT 22:30Wendy Chiridza
December 6, 2025 AT 07:06Pamela Mae Ibabao
December 7, 2025 AT 04:21Palanivelu Sivanathan
December 8, 2025 AT 02:14Jessica Ainscough
December 8, 2025 AT 06:23Kevin Estrada
December 8, 2025 AT 12:54Katey Korzenietz
December 9, 2025 AT 20:08Michael Bene
December 10, 2025 AT 17:23Brian Perry
December 11, 2025 AT 23:06Chris Jahmil Ignacio
December 13, 2025 AT 00:10Paul Corcoran
December 14, 2025 AT 06:36