Medication Dosing: How to Get It Right and Avoid Dangerous Mistakes
When you take a pill, medication dosing, the precise amount and timing of a drug given to achieve the desired effect without harm. Also known as drug dosage, it’s not just a number on a label—it’s the difference between healing and harm. Too little and the drug does nothing. Too much and you risk overdose, organ damage, or worse. Even when you’re taking a generic drug, a chemically identical version of a brand-name medication approved by the FDA, the dosing rules don’t change. A generic pill works the same way as the brand, but if you skip a dose, double up, or take it with the wrong food, you’re playing Russian roulette with your body.
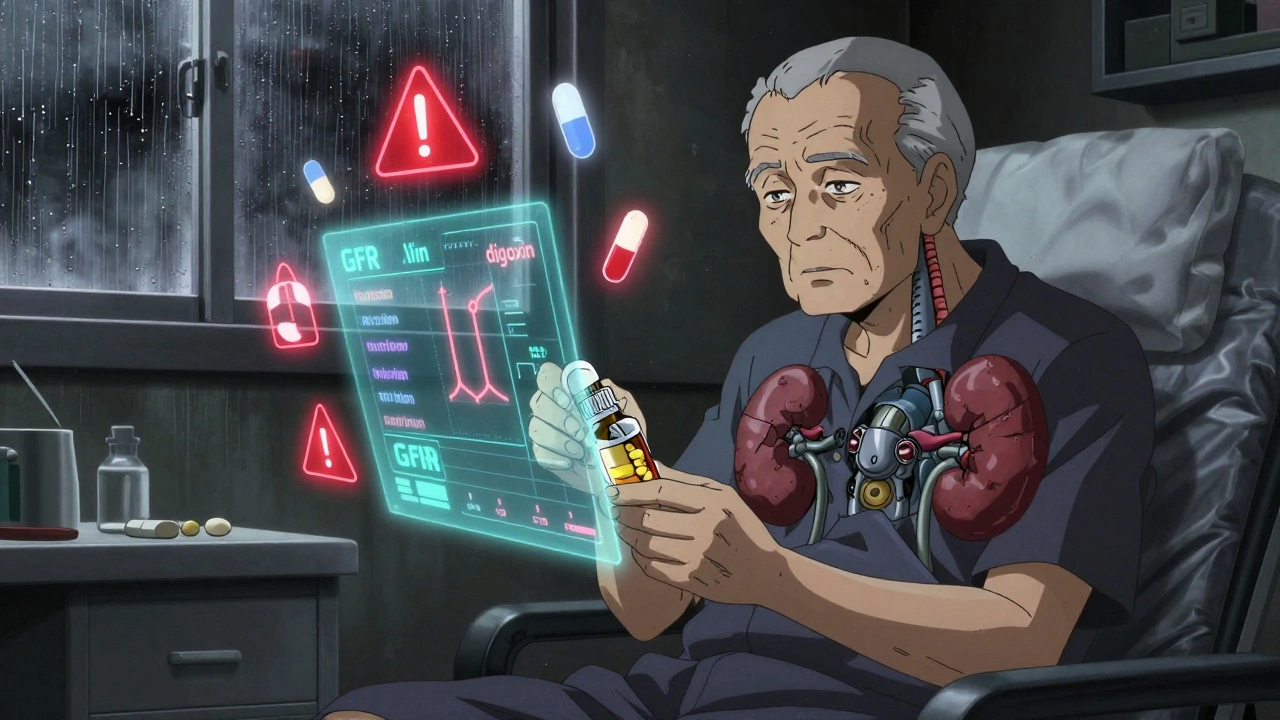
Why does dosing matter so much? Because your body doesn’t treat every drug the same. pharmacokinetic interactions, how your body absorbs, breaks down, and removes a drug can change based on what else you’re taking. Coffee, grapefruit juice, antacids, even certain supplements can alter how fast your liver processes a pill. That’s why mixing drug interactions, when two or more substances affect each other’s effects in the body—like yohimbe and blood pressure meds—can spike your heart rate or cause a stroke. And it’s not just about what you take together. Your age, weight, kidney function, and even your gut bacteria can change how a dose affects you. A dose that’s safe for a 30-year-old might be dangerous for a 75-year-old with reduced kidney function.
Many people think dosing is simple: take one pill a day. But what if your pill needs to be taken on an empty stomach? What if skipping one dose causes your blood pressure to rebound dangerously? What if you’re on warfarin and your doctor changes your dose because you started eating more kale? Medication dosing isn’t a one-size-fits-all formula. It’s a dynamic system that requires attention, communication, and sometimes, a second opinion. People with low vision or hearing loss face extra risks because pill labels are hard to read or pharmacists’ instructions are missed. Older adults with bloating from multiple meds might not realize their gas is a side effect of their heart drug, not just aging. And in hospitals, even a tiny dosing error can trigger a chain reaction—wrong dose, wrong time, wrong patient.
What you’ll find below isn’t just theory. It’s real-world guidance from people who’ve been there: how to avoid mixing dangerous supplements with your prescriptions, why generic drugs aren’t always interchangeable in practice, how to spot when a drug isn’t working because the dose is off, and what to do when your body reacts unexpectedly. From opioid overdose reversal with naloxone to managing insulin during illness, these posts give you the tools to take control—not guesswork, not fear, but clear, proven steps to keep your dosing safe and effective.