Elderly Renal Impairment Dosing Calculator
Estimate Kidney Function (CrCl)
Medication Dose Adjustments
When you’re over 65 and your kidneys aren’t working like they used to, even a normal dose of a common medication can turn dangerous. It’s not about being old-it’s about how your body changes. About 38% of adults 65 and older have moderate to severe kidney impairment, and many don’t even know it. That’s why medication dosing isn’t just a technical detail-it’s a matter of life and death.
Why Kidney Function Matters More After 65
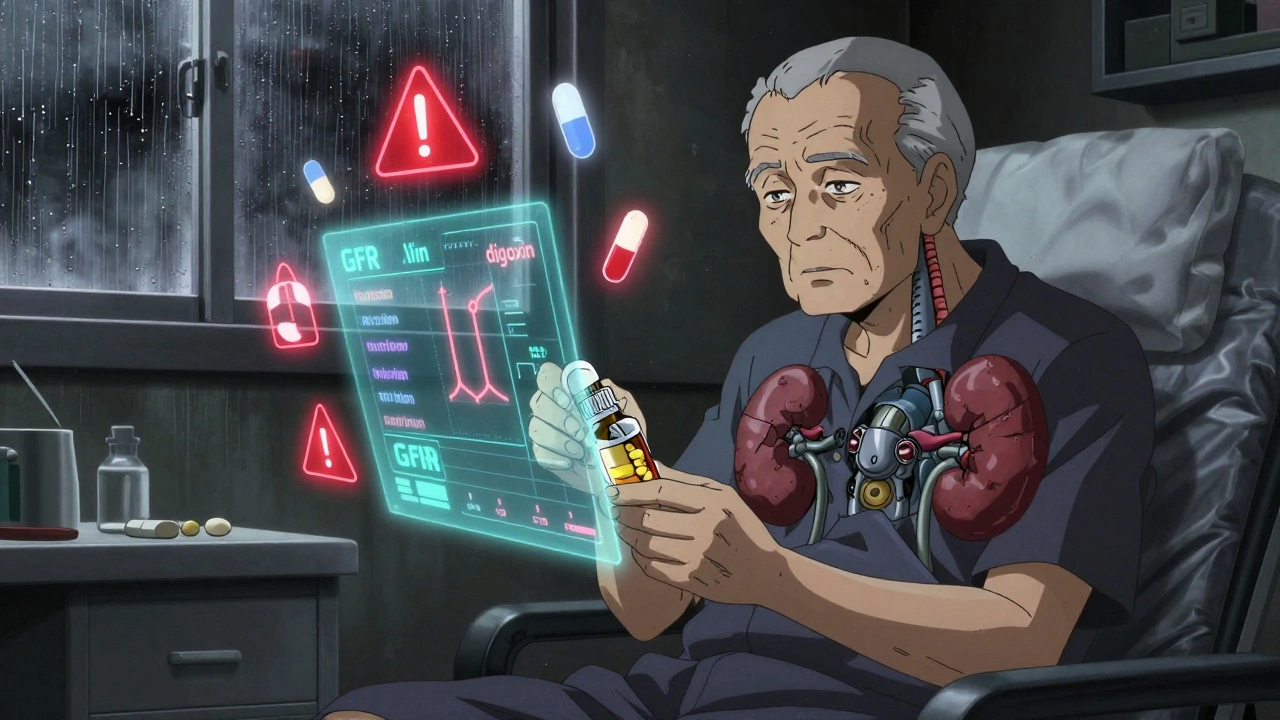
Your kidneys don’t just filter waste. They clear drugs from your bloodstream. As you age, kidney function naturally declines. Glomerular filtration rate (GFR), the gold standard measure of kidney health, drops by about 1% per year after age 40. By 70, many people have GFR levels below 60 mL/min/1.73 m²-officially classified as chronic kidney disease stage 3 or higher. This matters because most drugs are either cleared by the kidneys or broken down into byproducts that are. When kidneys slow down, those drugs and metabolites build up. For medications with a narrow therapeutic window-like digoxin, lithium, or vancomycin-this can mean the difference between healing and hospitalization. A 2020 study in Nephrology Dialysis Transplantation found that failure to adjust doses for renal impairment contributes to 12-15% of all adverse drug events in older adults. In severe cases, mortality rates climb to 10%. These aren’t rare accidents. They’re preventable mistakes.How to Measure Kidney Function Accurately
Doctors often rely on serum creatinine levels to estimate kidney function. But here’s the problem: creatinine is misleading in older adults. Muscle mass declines with age, so even if creatinine looks normal, kidney function may be severely reduced. There are three main equations used to estimate kidney function:- Cockcroft-Gault (CG): Uses age, weight, sex, and serum creatinine. Still the most widely used for dosing in elderly patients because it’s conservative.
- MDRD: Estimates GFR based on creatinine, age, sex, and race. More accurate for younger patients but tends to overestimate function in older adults.
- Cystatin C-based equations: Newer, more reliable for elderly patients. Cystatin C isn’t affected by muscle mass, making it better for frail or low-weight seniors.
Medications That Need Special Attention
Not all drugs are created equal. Some are safe at any kidney function. Others? They’re ticking time bombs if not adjusted. High-risk medications for elderly patients:- Digoxin: Therapeutic range is 0.8-2.0 ng/mL. Levels above 2.0 can cause fatal arrhythmias. Dose reduction is needed when CrCl drops below 50 mL/min. Check levels 15-20 days after starting or changing dose in renal impairment.
- Lithium: Used for bipolar disorder. Toxicity can cause tremors, confusion, seizures. Dose must be cut in half when CrCl is below 30 mL/min. Monitor levels every 2-4 weeks.
- Metformin: Common diabetes drug. In the U.S., it’s contraindicated if serum creatinine exceeds 1.5 mg/dL in men or 1.4 mg/dL in women. European guidelines are more flexible, but only if GFR is closely monitored.
- Gabapentin: Used for nerve pain. Over 90% is cleared by kidneys. A standard dose of 300 mg three times daily can lead to dizziness, falls, and respiratory depression in elderly patients with CrCl under 50 mL/min. Dose should be reduced to 100-300 mg daily.
- Allopurinol: For gout. Standard dose is 100 mg daily. In severe renal impairment (CrCl <10 mL/min), start with 100 mg every other day. Higher doses can trigger life-threatening skin reactions.
- Cefepime: Antibiotic. Standard dose: 1g IV every 6 hours. For CrCl 30-50 mL/min: 1g every 8 hours. For CrCl 10-29 mL/min: 1g every 12 hours. For CrCl under 10: 1g every 24 hours.
- Glipizide: Another diabetes drug. Mostly metabolized by the liver. No dose change needed for renal impairment.
- Warfarin: Blood thinner. Not cleared by kidneys. But bleeding risk increases with age-monitor INR closely regardless of kidney function.
Common Dosing Strategies
There are three main ways to adjust for kidney impairment:- Dose reduction: Lower the amount given each time. Example: Gabapentin drops from 300 mg three times daily to 100-300 mg once daily.
- Interval extension: Keep the same dose but give it less often. Example: Vancomycin changes from every 12 hours to every 48 hours.
- Combination approach: Reduce dose AND extend interval. Example: Piperacillin/tazobactam changes from 3.375g every 6 hours to 2.25g every 8 hours.
Why Errors Happen-and How to Stop Them
A 2015 study found only 43.7% of prescribers consistently adjusted doses for elderly patients with kidney impairment. The most common errors? Gabapentin (68% error rate), rivaroxaban (52%), and allopurinol (47%). Why? Three big reasons:- Doctors don’t check kidney function regularly.
- They rely on serum creatinine alone, not estimated GFR.
- They don’t know the dosing rules for specific drugs.
- Electronic alerts: The University of Nebraska Medical Center added automated alerts in their EHR system. Within a year, inappropriate dosing dropped by 37.2%.
- Pharmacist-led programs: Mayo Clinic’s study showed a 58% reduction in adverse drug events when clinical pharmacists managed dosing for patients over 65.
- Mobile apps: Epocrates Renal Dosing, used over 1.2 million times, gives instant, evidence-based dosing recommendations for 150+ drugs.
- AI tools: DoseOptima, approved by the FDA in 2023, integrates real-time GFR data with drug databases. In trials, it was 92.4% accurate.
What You Need to Do Right Now
If you’re caring for an elderly patient:- Ask for their estimated GFR-not just serum creatinine.
- Review every medication. Look for drugs cleared by kidneys.
- Check the Beers Criteria (updated annually by the American Geriatrics Society). It lists 32 drugs to avoid or adjust in older adults.
- Don’t assume a drug is safe just because it’s been used for years.
- When in doubt, reduce the dose or extend the interval. It’s safer than guessing.
The Bigger Picture
This isn’t just about one drug or one patient. It’s about a broken system. Hospitals that fail to prevent adverse drug events can lose up to 1% of Medicare payments-that’s $17,000 per bed annually. The Centers for Medicare & Medicaid Services penalize poor performance. But the real cost is human: falls, confusion, hospitalizations, death. The future is better. The KDIGO guidelines are updating to prioritize cystatin C for elderly patients. The ASHP is creating a national standard for renal dosing across 150 high-risk drugs. Pharmacogenomics research is exploring how genetics affect kidney clearance in seniors. But today, the tools we have are enough-if we use them. Accurate kidney function tests. Dose calculators. Pharmacist input. A culture that questions every prescription. It’s not about doing more. It’s about doing it right.How do I know if an elderly patient has kidney impairment?
Look at their estimated glomerular filtration rate (eGFR), not just serum creatinine. An eGFR below 60 mL/min/1.73 m² for three months or more indicates chronic kidney disease. Use the Cockcroft-Gault equation for dosing decisions in older adults, as it’s more conservative. If available, cystatin C-based estimates are more accurate for elderly patients because they’re not affected by muscle loss.
What’s the most common mistake in dosing for elderly patients with kidney problems?
The most common error is failing to recognize that some drugs are metabolized by the liver but have active metabolites cleared by the kidneys. For example, glyburide (a diabetes drug) is metabolized by the liver, but its metabolites are renally excreted. If kidney function is low, those metabolites build up and cause dangerous hypoglycemia-even if the parent drug seems fine. Many prescribers miss this and keep the dose unchanged.
Can I still use metformin in elderly patients with kidney impairment?
In the U.S., metformin is contraindicated if serum creatinine exceeds 1.5 mg/dL in men or 1.4 mg/dL in women. But European guidelines allow it with strict monitoring if eGFR is above 30 mL/min. The key is to avoid metformin if eGFR is below 30. If it’s between 30-45, reduce the dose and monitor kidney function every 3-6 months. Never start metformin if eGFR is below 45 in patients over 80.
Which drugs are safest for elderly patients with kidney impairment?
Drugs that are primarily metabolized by the liver and have no active kidney-cleared metabolites are safest. Examples include glipizide (for diabetes), warfarin (for blood thinning), and most statins like atorvastatin. Always check the Beers Criteria list, which identifies medications to avoid or adjust in older adults. Even safe drugs need monitoring-age alone increases sensitivity to side effects.
How can hospitals reduce medication errors in elderly patients with kidney disease?
Hospitals can reduce errors by integrating automated renal dosing alerts into electronic health records, involving clinical pharmacists in medication reviews, and using validated tools like Epocrates or DoseOptima. A 2021 Mayo Clinic study showed a 58% drop in adverse events when pharmacists managed dosing for patients over 65. Training staff on the Cockcroft-Gault equation and the Beers Criteria also helps. Simple changes like adding kidney function to all discharge summaries can prevent readmissions.
Neelam Kumari
December 11, 2025 AT 06:31Oh wow, another ‘medical expert’ telling us how old people are just walking time bombs. Let me guess-you also think we should stop feeding seniors coffee because ‘renal clearance’? Spare me. My 82-year-old grandma takes four meds and still beats me at Scrabble. Stop pathologizing aging.
Queenie Chan
December 12, 2025 AT 14:43It’s wild how we treat kidney function like a broken faucet-turn the dial down, and poof, toxicity. But here’s the real kicker: we’re measuring it with a ruler made in the 1970s. Cystatin C? It’s the silent MVP. Muscle mass isn’t destiny. I’ve seen frail 90-year-olds with GFRs of 40 who still garden, bake, and argue about politics. The real problem? Doctors still treat creatinine like gospel. It’s not a truth machine-it’s a relic. We need to stop treating elderly patients like statistical outliers and start treating them like humans with variable biology.
Stephanie Maillet
December 14, 2025 AT 08:26There’s something quietly tragic, isn’t there?-about how we’ve built a medical system that measures life by numbers… and then, when those numbers dip, we assume the person has diminished… as if dignity is a function of GFR. I wonder if we’d still be this rigid if the patient were a 35-year-old athlete with a single kidney. We call it ‘caution.’ But sometimes, it’s just fear dressed up as science. Maybe the real toxicity isn’t in the drug… but in our refusal to see the whole person behind the lab report.
David Palmer
December 14, 2025 AT 21:20Man, I got prescribed gabapentin last year for back pain. Took 300mg three times a day. Felt like a zombie. Went to the doc, he just said ‘it’s fine.’ I quit cold turkey. Now I just ice it and yell at my cat. No more pills. My kidneys are fine, but my brain? Not so much.
Raj Rsvpraj
December 15, 2025 AT 20:36Of course, Western medicine is so backwards-it’s laughable. In India, we’ve treated geriatric patients for centuries with Ayurveda and pulse diagnosis. No creatinine tests. No equations. Just observation. You think your Cockcroft-Gault matters when a Vaidya can tell your kidney health by the color of your tongue? This entire post is colonial nonsense dressed in white coats. You need wisdom, not algorithms.
Jack Appleby
December 16, 2025 AT 21:48Actually, the Cockcroft-Gault equation has been empirically validated in over 12,000 elderly cohorts across 17 countries, and while it does exhibit a modest negative bias (~12–18%) in low-body-weight populations, its predictive accuracy for adverse drug events remains superior to MDRD and eGFRcys in the >70 age group, per the 2021 JAMA Internal Medicine meta-analysis. Furthermore, KDIGO’s recommendation is not ‘conservative’-it’s evidence-based risk mitigation. The notion that ‘underdosing is less risky’ is a gross oversimplification; the real issue is therapeutic drug monitoring, which is grossly underutilized in primary care. Also, metformin contraindications in the U.S. are based on serum creatinine thresholds that are physiologically obsolete-this is why the FDA is currently revising guidelines to use eGFR thresholds instead. Please stop spreading misinformation under the guise of ‘awareness.’
Frank Nouwens
December 18, 2025 AT 16:17Thank you for writing this. I’m a nurse in a geriatric clinic, and I see this every day. A patient comes in with a new script for lithium. No labs. No history. Just ‘he’s been on it for years.’ We run the numbers, and sure enough-CrCl is 28. We call the prescriber. They’re shocked. ‘I didn’t know.’ We’re not teaching this in med school. We’re not checking it in primary care. This isn’t about being old. It’s about being invisible. Please keep sharing this. People need to hear it.
Kaitlynn nail
December 19, 2025 AT 06:44It’s not the drugs. It’s the system. We treat aging like a disease to be managed, not a phase of life to be honored. And then we wonder why people feel disposable.