Geriatric Pharmacology: How Medications Work for Older Adults
When we talk about geriatric pharmacology, the study of how drugs affect older adults and how their bodies change the way medicines work. It's not just about giving smaller doses—it's about understanding how aging reshapes every step of how a drug moves through the body, from absorption to elimination. People over 65 take an average of four to five prescription drugs daily. That’s not because they’re sick more often—it’s because their bodies no longer handle meds the same way they did at 30.
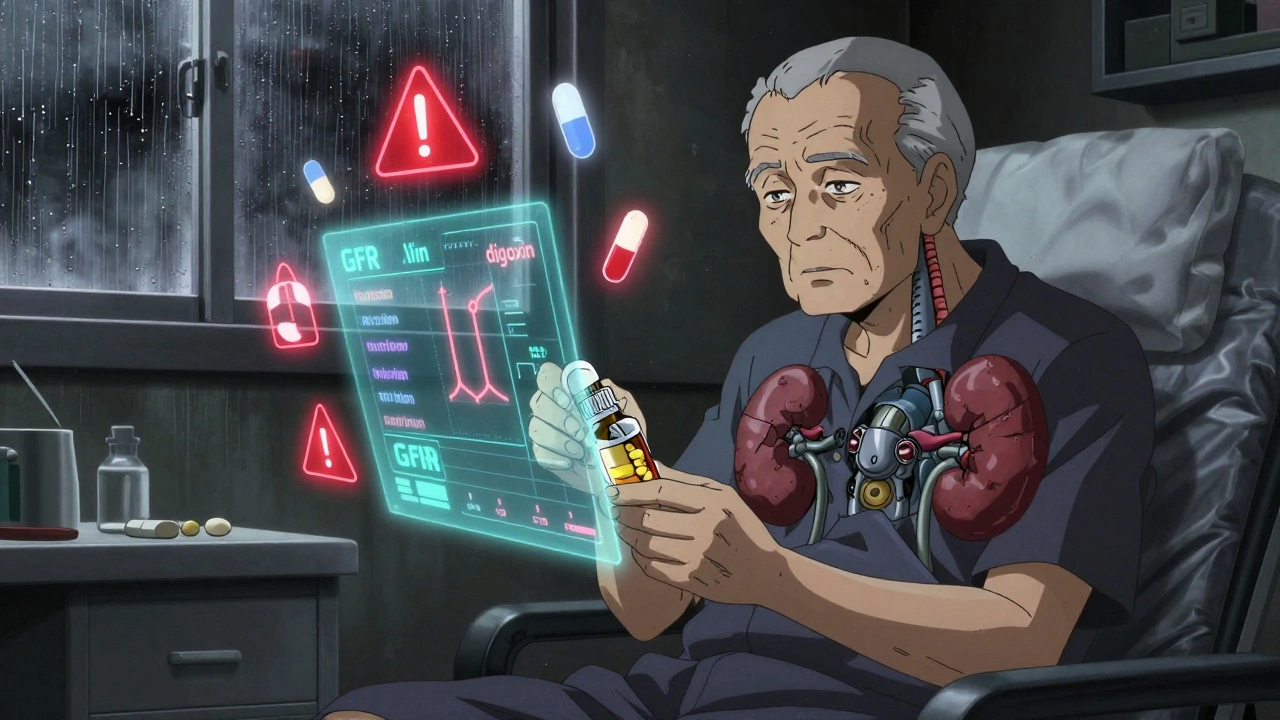
polypharmacy, the use of multiple medications at once is common in older adults, but it’s also one of the biggest risks. A pill for blood pressure, another for arthritis, a third for sleep, and maybe a supplement on top—that’s a recipe for hidden clashes. One drug might slow down how fast another is broken down, causing it to build up to toxic levels. Or two meds might both lower blood pressure so much that dizziness and falls become likely. drug interactions in seniors, when two or more medications affect each other’s effects or safety in older bodies don’t always show up in warning labels. They’re silent, slow, and often mistaken for normal aging.
age-related drug metabolism, how the liver and kidneys change with age, affecting how quickly drugs are processed is the hidden engine behind many problems. Your liver gets slower. Your kidneys filter less. Fat increases, water decreases. That means a drug meant for a 50-year-old might stay in a 75-year-old’s system twice as long. Even a safe dose can become dangerous. And it’s not just about the pills themselves—some over-the-counter meds, supplements like yohimbe, or even grapefruit juice can throw everything off balance.
Geriatric pharmacology isn’t just for doctors. It’s for anyone managing meds for themselves or a loved one. It’s about asking: Does this still make sense? Is there a simpler way? Are we treating a symptom or creating a new problem? The posts below dig into real-world cases: how heart failure drugs change in older patients, why statins cause muscle pain more often with age, how kidney function affects blood thinners, and why a medication that worked fine at 60 might cause confusion at 80. You’ll find practical tips on spotting dangerous combinations, understanding why generics are often the smart choice, and how to talk to your pharmacist about what’s really in your medicine cabinet.