Generic Drug Safety: What You Need to Know About Quality, Cost, and Real-World Use
When you hear generic drug safety, the assurance that off-brand medications meet the same standards as name-brand versions. Also known as generic medications, they are the backbone of affordable healthcare in the U.S. and beyond. Many people worry that cheaper means weaker, but the truth is simpler: if a generic drug is approved by the FDA, it must contain the same active ingredient, work the same way in your body, and meet the same strict quality controls as the brand-name version. There’s no hidden catch—just lower prices because companies don’t need to spend millions on advertising or re-inventing a drug already proven to work.
One of the biggest concerns around generic drugs, medications that are chemically identical to brand-name drugs but sold under their chemical name is whether they’re truly interchangeable. The answer is yes—for nearly all cases. The FDA approval, the rigorous process that ensures generic drugs are bioequivalent to their brand-name counterparts means every batch is tested for strength, purity, and how quickly it dissolves in your system. You won’t find a generic version on shelves unless it matches the brand within a 3-5% margin of performance. That’s tighter than many food and beverage standards. What changes? The inactive ingredients—fillers, dyes, coatings. These can sometimes cause minor differences in how a pill feels or tastes, but never in how it treats your condition.
Still, questions come up. What about drug interactions, when two or more medications affect each other’s effects in the body? The good news is, generic drugs don’t introduce new interaction risks. If your brand-name blood pressure pill interacts with grapefruit juice, so does its generic twin. The same goes for brand name drugs, medications sold under a trademarked name, often at higher prices due to marketing and patent protection. The difference isn’t in how they behave in your body—it’s in the price tag. Generics cost up to 85% less because competition drives prices down after patents expire. No magic. No shortcuts. Just smart regulation and market forces.
Some people report feeling different after switching—more side effects, less relief. But studies show this is often psychological. When you switch from a familiar blue pill to a white one, your brain can trick you into thinking something’s wrong. That’s why clear labeling, patient education, and pharmacist guidance matter so much. The generic drug safety system works when you trust it. And it’s trusted by doctors, insurers, and over 90% of U.S. prescription fills for good reason.
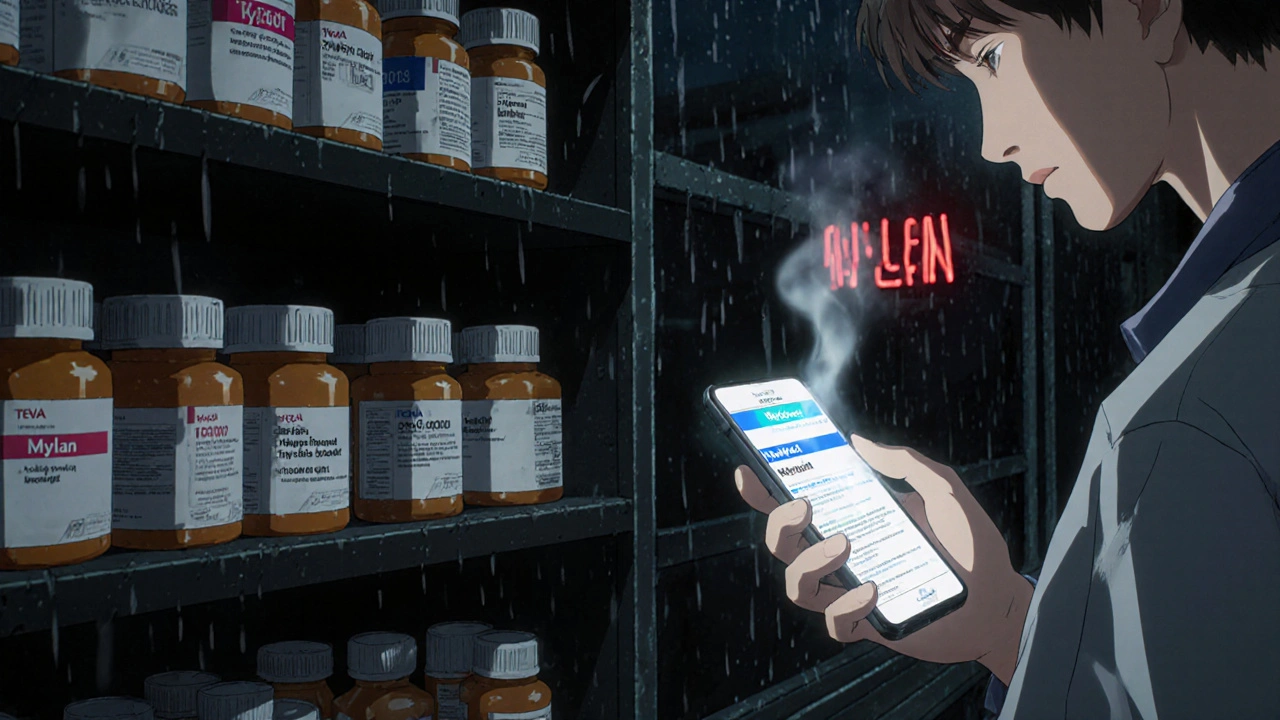
Below, you’ll find real stories and data-backed guides that cut through the noise. From how patent lawsuits delay access to why some people tolerate generics better than others, to how digital pharmacies are making these drugs easier to get—every post here is built to help you make confident, informed choices without overpaying or second-guessing your meds.