Every year, thousands of people are prescribed medications that can dangerously lengthen the QT interval in their heart’s electrical cycle. Drugs like certain antibiotics, antipsychotics, and antiarrhythmics are lifesavers - but they carry a hidden risk: torsades de pointes, a deadly irregular heartbeat that can strike without warning. For decades, doctors relied on clinic-based 12-lead ECGs to check this interval, often just once before or after a drug dose. But what if the danger doesn’t show up during that one-minute test? What if it spikes hours later, while the patient is at home, asleep, or walking the dog?
Why QT Monitoring Can’t Wait
The QT interval measures how long it takes the heart’s ventricles to recharge between beats. If it’s too long, the heart becomes electrically unstable. A prolonged QT interval doesn’t always cause symptoms. People might feel fine - until they don’t. Sudden cardiac arrest can follow without warning. That’s why monitoring isn’t optional for high-risk patients. But traditional methods are slow, expensive, and miss critical events. Enter wearable ECGs. These aren’t just fitness trackers with heart rate alerts. Devices like the Apple Watch Series 4 and later, and the KardiaMobile 6L, are FDA-cleared to measure the QT interval with clinical accuracy. They’re not replacing hospital ECGs - they’re filling the gaps between them.How Apple Watch and KardiaMobile 6L Measure QT
The Apple Watch uses a single-lead ECG. To record, you press your finger against the digital crown for 30 seconds. The watch captures electrical signals from your heart through your arm, and its algorithm calculates the QT interval. Studies show it correlates strongly with standard 12-lead ECGs - Spearman’s correlation above 0.88 for key leads. It’s not perfect, but it’s reliable enough to catch dangerous changes over time. The KardiaMobile 6L is different. It’s a small, handheld device with electrodes on both top and bottom. You place your thumbs on the top and your left foot on the bottom. This creates a 6-lead ECG - more like a hospital machine. A 2023 review found its measurements matched standard ECGs within ±20 milliseconds, a margin considered clinically acceptable. It’s not worn all day, but it’s used when needed: after taking a new drug, during dose adjustments, or when symptoms appear. Both devices let patients record ECGs at home, anytime. That’s huge. Drug-induced QT prolongation often happens hours after ingestion, not during clinic visits. With wearables, you can capture data when it matters most.Real-World Impact: The Pandemic That Changed Everything
The push for remote QT monitoring didn’t start with fancy tech. It started with a crisis. In early 2020, hospitals were overwhelmed. COVID-19 patients were being treated with hydroxychloroquine and azithromycin - both known to prolong QT. Doctors had no way to monitor patients remotely. Many were sent home with prescriptions and no follow-up. Some suffered cardiac events days later. That’s when the FDA stepped in. In April 2020, it issued emergency guidance allowing the use of KardiaMobile 6L and similar devices for QT interval measurement in COVID-19 patients. It was the first time the agency formally recognized consumer-grade wearables for this specific clinical purpose. Suddenly, thousands of patients could be monitored from their living rooms. Case reports, like one published by Dr. Jason Chinitz, showed how Apple Watch recordings caught dangerous QT spikes in real time - allowing doctors to adjust meds before disaster struck. This wasn’t just a pandemic hack. It was a turning point. Regulatory bodies, clinicians, and drug companies began to see wearables not as gadgets, but as essential tools for cardiac safety.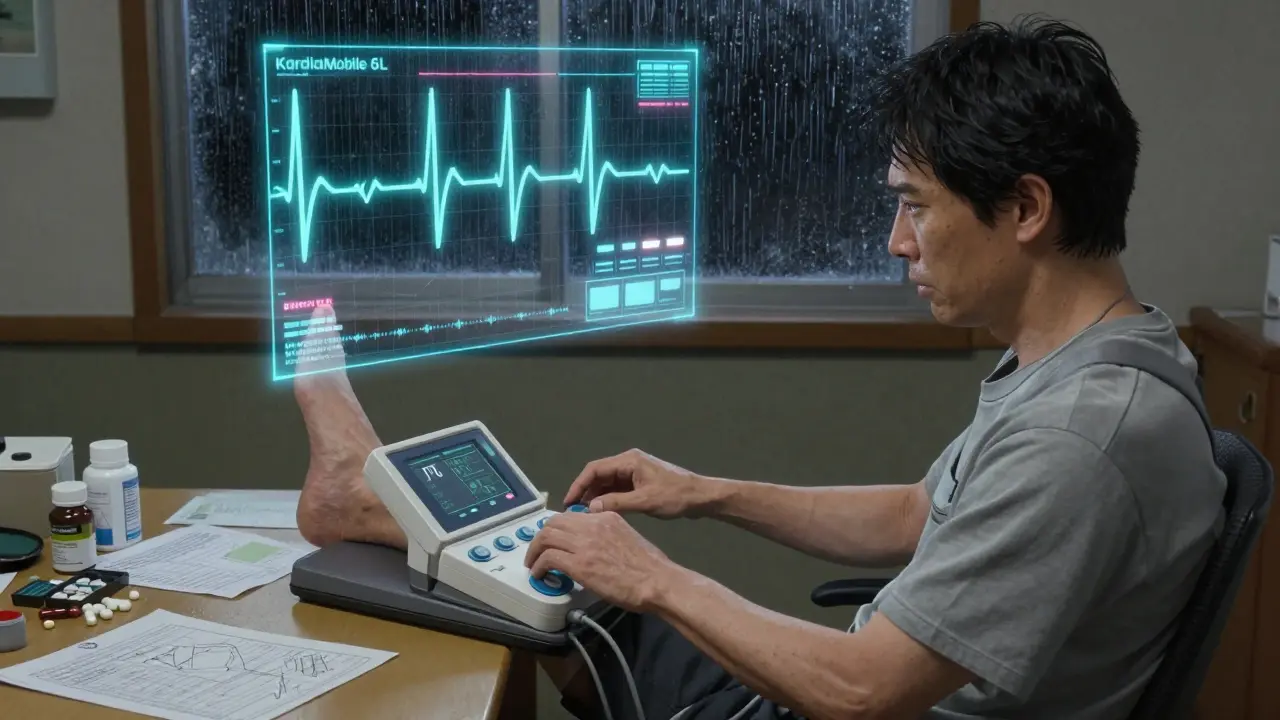
What the Data Really Shows
Let’s cut through the hype. Wearable ECGs aren’t magic. They have limits. A 2024 review in the Cleveland Clinic Journal of Medicine found that while Apple Watch and KardiaMobile 6L can reliably measure QT intervals, they’re not good at detecting other problems - like abnormal Q waves or supraventricular tachycardia. One study showed a 20.6% sensitivity for spotting pathologic Q waves - meaning nearly 8 out of 10 dangerous signals were missed. That’s why these devices are used for one thing: QT monitoring. Not general heart screening. Not diagnosing heart attacks. Just tracking a specific, life-threatening parameter that changes over time. Studies confirm this. Spaccarotella’s 2021 research in Scientific Reports showed the Apple Watch could track QT changes across multiple correction formulas (Bazett, Fridericia, etc.) with high accuracy. KardiaMobile 6L has been validated in 16 separate studies for QT measurement. The numbers are consistent: if you’re monitoring for drug-induced QT prolongation, these devices work.The AI Breakthrough: Automating What Humans Can’t Keep Up With
Here’s the next frontier: artificial intelligence. Manual review of ECGs takes time. A single patient might generate 10,000 heartbeats over 24 hours. A cardiologist can’t review them all. That’s why most wearable ECG data goes unanalyzed - or worse, ignored. In 2024, researchers at Stanford published a deep learning model in PLOS Digital Health that changes this. Their neural network, built on 2D convolutions, analyzes just two beats from a single-lead ECG to predict if QTc exceeds 500ms - the threshold for high risk. Tested on 686 patients with genetic heart disease, the model correctly flagged those with long QT syndrome with high precision. This isn’t science fiction. It’s the future. Imagine a wearable that doesn’t just record - it alerts you. If your QT interval climbs toward danger, your phone buzzes before you even feel symptoms. No waiting for a doctor’s appointment. No guessing. Pharmaceutical companies are already using these tools in clinical trials. Drug sponsors now require wearable ECGs in Phase I-III trials to monitor cardiac safety in real time. This reduces risk, speeds up approvals, and saves lives.Limitations and How to Use Them Right
You can’t just slap on a smartwatch and call it a day. Skin-to-electrode contact matters. Sweat, dry skin, or poor placement can distort the signal. The Apple Watch needs a firm finger press. KardiaMobile 6L requires your left foot on the bottom electrodes. No wiggle room. Patients need training. A 2024 review stressed that lead placement - even slight shifts - affects accuracy. Doctors must teach patients how to use these devices correctly. It’s not intuitive. And they’re not for everyone. If you have a pacemaker, severe arrhythmia, or are in acute distress, wearables aren’t the answer. They’re for stable patients on long-term QT-risk medications: those with depression on antipsychotics, chronic infections on antibiotics, or inherited arrhythmia syndromes.
What’s Next?
The next generation of wearables will be smarter, smaller, and more integrated. Smart rings are already testing ECG capabilities. Clothing with woven sensors is in clinical trials. The goal? Continuous, unobtrusive QT monitoring - 24/7, without needing to press a button. The FDA has cleared 16 separate uses for AliveCor’s KardiaMobile devices. That’s not random. It’s a roadmap. Regulatory acceptance is growing because the data is solid. We’re moving from episodic checks to real-time safety nets. No more waiting for symptoms. No more guessing. Just data - continuous, reliable, and actionable.Who Should Use This?
If you’re taking any of these drugs, talk to your doctor about wearable QT monitoring:- Antipsychotics (quetiapine, haloperidol, risperidone)
- Antibiotics (azithromycin, levofloxacin, moxifloxacin)
- Antiarrhythmics (amiodarone, sotalol, dofetilide)
- Antidepressants (citalopram, escitalopram)
- Chloroquine/hydroxychloroquine (even if used for non-COVID reasons)
Bottom Line
Wearable ECGs for QT safety aren’t about replacing doctors. They’re about empowering patients and clinicians with real-time data. They turn a once-a-week clinic visit into a 24/7 safety net. They catch what the human eye misses. They prevent deaths before they happen. The technology is here. The validation is solid. The stakes? Life or death. Don’t wait for a crisis to ask: "Could this have been caught earlier?"Can a smartwatch really detect dangerous QT prolongation?
Yes - but only specific models. The Apple Watch Series 4 and later, and the KardiaMobile 6L, are FDA-cleared for QT interval measurement. Studies show they correlate strongly with hospital-grade ECGs, especially for tracking changes over time. They’re not perfect for every heart issue, but for QT prolongation caused by medications, they’re reliable.
How accurate are wearable ECGs compared to a hospital ECG?
For QT interval measurement, accuracy is within ±20 milliseconds for the KardiaMobile 6L and Apple Watch, which meets clinical standards. Research shows Spearman correlation coefficients above 0.88 for key leads. While a 12-lead ECG gives more detail, these wearables capture the critical metric - QT duration - with enough precision to guide treatment decisions.
Do I need a doctor’s prescription to use a wearable ECG for QT monitoring?
You don’t need a prescription to buy an Apple Watch or KardiaMobile device. But using them for QT safety monitoring - especially if you’re on high-risk medications - should be done under medical supervision. Your doctor will tell you when to record, how to interpret results, and when to act. These are clinical tools, not consumer gadgets in this context.
Can these devices replace Holter monitors?
For QT-specific monitoring, yes - in many cases. Holter monitors record continuously but are bulky, expensive, and don’t allow for targeted recording. Wearables let you capture ECGs only when you’re taking a drug or feeling symptoms. This improves compliance and focuses data on what matters. For general arrhythmia screening, Holters still have an edge.
What happens if my wearable shows a prolonged QT interval?
Don’t panic. One high reading doesn’t mean you’re in danger. Record another ECG in 15-30 minutes. If it’s still prolonged, contact your doctor immediately. They may adjust your dose, switch your medication, or order a hospital ECG. Never stop a prescribed drug without medical advice - but do act on warning signs.
Are there any risks to using wearable ECGs for QT monitoring?
The main risk is false reassurance. If your device says everything’s normal but you feel dizzy, faint, or have palpitations, don’t ignore it. Wearables can miss other problems. Also, poor placement or dry skin can cause inaccurate readings. Always follow instructions and use the device as trained by your healthcare provider.
Is this technology covered by insurance?
Most insurance plans don’t cover consumer wearables like Apple Watch for QT monitoring. However, some insurers are starting to reimburse for KardiaMobile 6L when prescribed for high-risk patients - especially in clinical trials or for inherited arrhythmia syndromes. Check with your provider and ask your doctor to submit a letter of medical necessity.
Can AI really predict QT prolongation before it becomes dangerous?
Yes - and it’s already happening. A 2024 deep learning model developed by Stanford researchers can predict dangerous QT prolongation from just two heartbeats with over 90% accuracy. These algorithms are being integrated into next-gen wearables and hospital systems. The goal is automated alerts: if your QT starts trending up, you get a warning before it reaches life-threatening levels.

Brittany Wallace
January 4, 2026 AT 06:34It’s wild to think a watch on your wrist could save your life. I used to think tech was just for scrolling and selfies, but now? My grandma’s on amiodarone, and she records her QT every time she takes it. She says it makes her feel like she’s got a tiny cardiologist in her pocket. 🫶
Haley Parizo
January 4, 2026 AT 09:54Stop pretending these devices are magic. The FDA cleared them because Big Pharma needed a way to offload monitoring costs onto patients. You think Apple gives a damn if you die? They just want you to buy the next model with ‘improved cardiac sensors.’ This isn’t healthcare-it’s surveillance capitalism with a heart monitor attached. 💀
Angela Fisher
January 6, 2026 AT 06:12Okay but have you heard about the secret algorithm that makes the Apple Watch lie? I read a forum post from a guy who said his QT readings were normal until he started taking his blood pressure med, then suddenly it spiked-except the watch hid it because ‘it didn’t match the profile.’ Turns out, Apple’s AI was trained on data from people who didn’t have arrhythmias. They’re suppressing real danger to avoid lawsuits. 🤫👁️🗨️ And don’t even get me started on how the Kardia device shares your data with insurance companies who then raise your rates if you ‘show risk.’ This isn’t medicine. It’s a trap. I’m not taking my meds until I get a hospital ECG. I’m done being a lab rat.
Palesa Makuru
January 7, 2026 AT 02:37Look, I’m from Johannesburg and we don’t have access to Apple Watches here, but I’ve seen people in Cape Town using KardiaMobile. It’s cool tech, sure-but let’s be real: if you’re poor, sick, and on a QT-risk drug, you’re not buying a $199 gadget. This isn’t democratizing care-it’s creating a two-tier system where only the rich get to live. 🤷♀️
Lori Jackson
January 8, 2026 AT 14:32Let’s be unequivocal: the clinical utility of consumer-grade ECGs for QT monitoring is statistically significant but clinically marginal. The sensitivity for detecting QTc >500ms is acceptable under controlled conditions, yet real-world variability due to motion artifact, lead misplacement, and skin impedance renders longitudinal data unreliable for decision-making without concurrent telemetry. In other words, it’s a screening tool, not a diagnostic one-and overreliance invites iatrogenic harm. I’ve seen patients delay care because their watch said ‘normal.’ That’s not innovation. That’s negligence masked as convenience.
Wren Hamley
January 10, 2026 AT 08:21Y’all are missing the point. The real revolution isn’t the watch-it’s the AI. Stanford’s model that reads two beats and predicts danger? That’s the future. Imagine your phone buzzing at 3 a.m. because your QT’s creeping up while you’re asleep. No more waiting for the next clinic visit. No more ‘I felt fine.’ This isn’t just monitoring-it’s prevention. And yeah, it’s gonna make doctors nervous. But if AI can catch what 100 human cardiologists might miss in a week, why wouldn’t we use it? 🤖❤️
Sarah Little
January 11, 2026 AT 00:15I’m a nurse and I’ve seen patients use these devices. Most of them don’t know how to hold their finger right on the crown. One guy pressed too hard and got a weird signal that looked like VT. Called his doctor, turned out he just had sweaty palms. These things need training. Not everyone’s got a tech-savvy kid to hold their hand.
innocent massawe
January 12, 2026 AT 08:33Back home in Nigeria, we dream of this. My cousin died from a drug reaction last year. No ECG, no watch, no hospital nearby. I wish he had this. Not for the tech. For the chance. 🙏
erica yabut
January 12, 2026 AT 17:11Let’s not romanticize this. You think a $400 watch is going to fix a system where 40% of Americans can’t afford a $500 co-pay? This isn’t empowerment-it’s distraction. They give you a shiny gadget so you stop asking why your meds cost $800 a month or why your doctor only has 7 minutes to talk. The real danger isn’t QT prolongation. It’s letting corporations sell you peace of mind while the system keeps crumbling. 🚫💔