What Is Thyroid Eye Disease?
Thyroid Eye Disease (TED), also called Graves’ ophthalmopathy, is an autoimmune condition where the body’s immune system attacks the tissues behind the eyes. It’s most common in people with Graves’ disease - an autoimmune disorder that causes an overactive thyroid - but it can also happen in those with normal or underactive thyroid function. About half of all Graves’ patients develop some form of TED, and it affects roughly 16 out of every 100,000 people each year. Women are four to six times more likely to get it than men, and it usually shows up between ages 40 and 60.
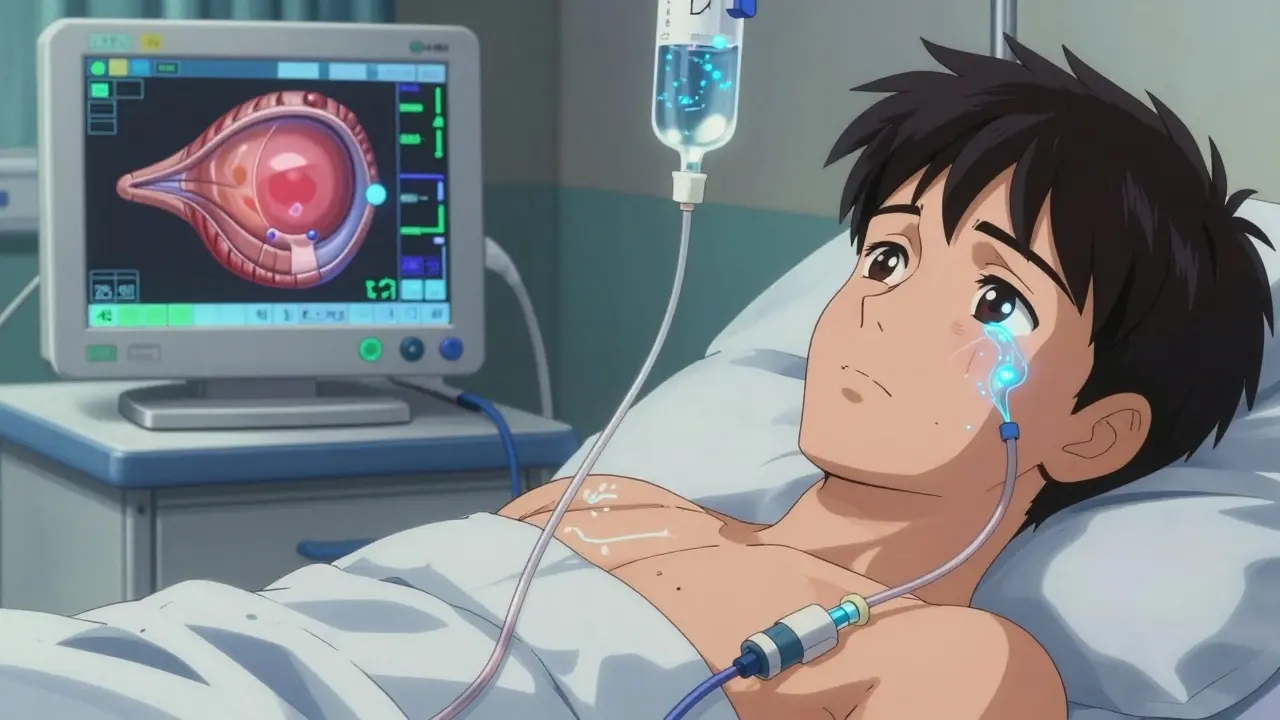
The real problem isn’t the thyroid itself - it’s what happens behind the eyes. Immune cells target fat and muscle tissue in the eye socket, causing inflammation, swelling, and fluid buildup. This pushes the eyeball forward, makes eyes red and puffy, and can mess with vision. The condition usually comes in two phases: an active, inflamed stage that lasts 6 to 24 months, and then a quieter, scarred stage where damage becomes permanent if not treated early.
Common Symptoms of Thyroid Eye Disease
If you’ve been told your eyes feel like they’re full of sand, you’re not imagining it. A gritty, burning sensation affects 78% of people with TED. Other signs include:
- Red, swollen eyelids and conjunctiva (the clear tissue covering the white of the eye)
- Light sensitivity and excessive tearing
- Pain behind the eyes, especially when moving them
- Dry eyes or a feeling that something’s stuck in your eye
- Forward bulging of the eyeballs (proptosis) - seen in about one-third of cases
- Double vision when looking side to side or up and down
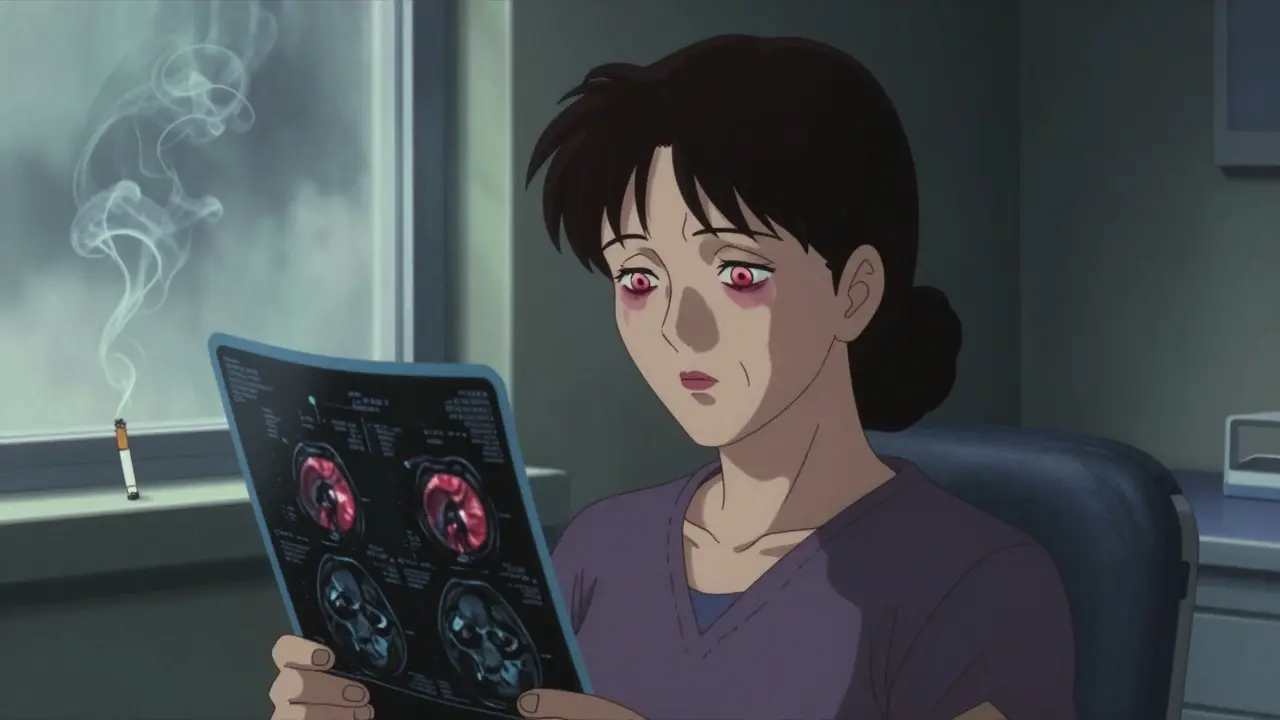
Most people (89%) get symptoms in both eyes, but 11% notice it in just one. The severity is measured using something called the Clinical Activity Score (CAS). If your score is 3 or higher, your disease is still active and needs treatment right away. Imaging tests like CT or MRI scans often show swollen eye muscles - especially the ones that move the eye downward and inward.
Why Smoking Makes TED Worse
If you smoke and have Graves’ disease, your risk of developing TED jumps by nearly eight times. Smoking doesn’t just make the disease more likely - it makes it worse. Smokers tend to have more severe swelling, more double vision, and respond poorly to treatment. Quitting smoking is one of the most effective things you can do to slow down TED, even before starting any medication. Studies show that people who quit during the early stages have much better outcomes than those who keep smoking.
Another big risk factor is high levels of TSH receptor antibodies (TRAb). If your TRAb level is above 15 IU/L, you’re nearly five times more likely to develop serious TED. That’s why doctors now test for these antibodies in every Graves’ patient - not just to manage the thyroid, but to predict eye problems before they start.
Steroids: The First-Line Treatment
When TED is active and inflamed, steroids are often the first treatment doctors reach for. The most effective version is intravenous methylprednisolone, given as a weekly infusion. The standard dose is 500 mg for six weeks, then 250 mg for another six weeks. This approach works in 60-70% of patients with moderate to severe disease, reducing swelling, redness, and double vision.
Oral prednisone is an alternative, but it’s less effective and comes with more side effects. People on daily pills often gain weight (an average of 8.2 kg), develop high blood sugar, or lose bone density. About a quarter of patients relapse once the dose is lowered. That’s why IV steroids are preferred - they deliver more drug directly to the inflamed tissue with fewer systemic effects.
Doctors limit the total IV dose to about 4.5-5 grams to avoid rare but serious liver damage. Even with that safety net, some patients still feel tired, get hot flashes, or notice a metallic taste during infusions. But compared to the risk of permanent vision loss, most agree it’s worth it.
Biologics: A New Era in TED Treatment
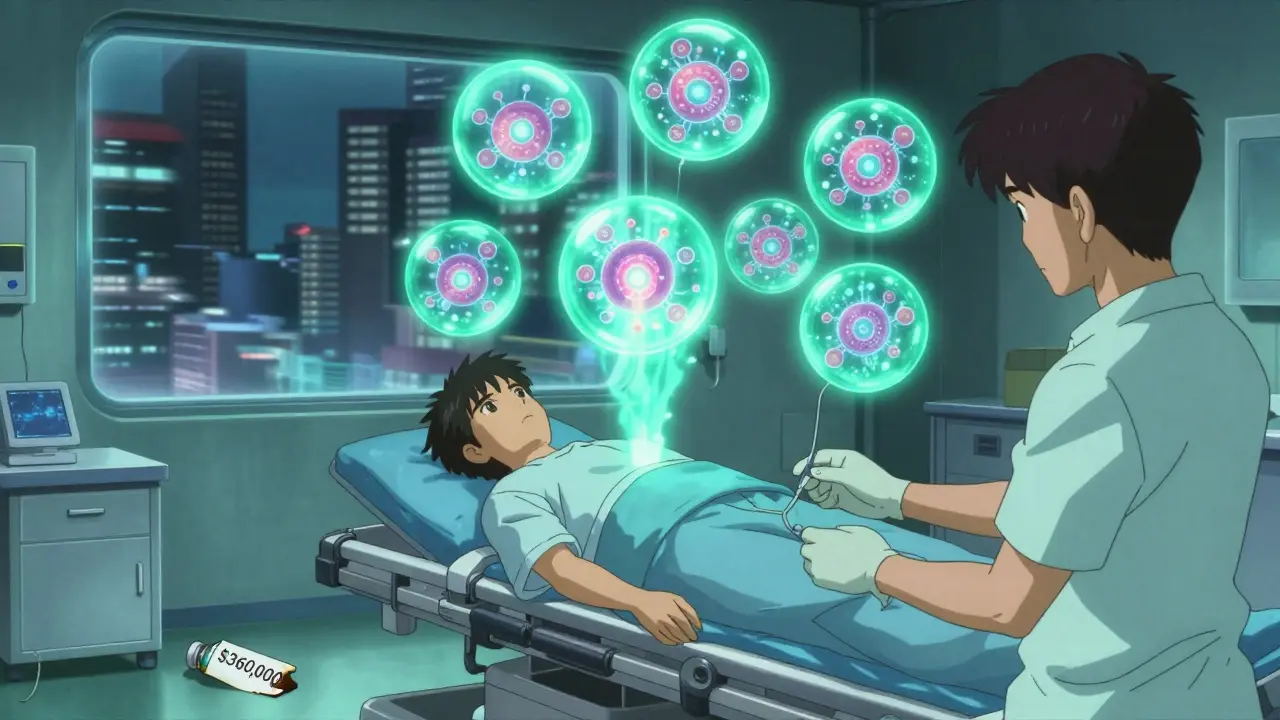
In 2020, the FDA approved teprotumumab (brand name Tepezza®), the first drug designed specifically to treat TED at its source. Unlike steroids, which just suppress inflammation, teprotumumab targets the insulin-like growth factor-1 receptor (IGF-1R), which is overactive in TED tissue. This stops the immune attack before it causes more damage.
In the OPTIC clinical trial, 71% of patients saw their eyeballs pull back by at least 2 millimeters - a huge change for someone who can’t close their eyes fully or feels like they’re always staring. Nearly 60% had their double vision improve, compared to just 26% on placebo. The treatment involves eight infusions over 24 weeks, given every three weeks.
But there’s a catch: it costs about $360,000 per course. Insurance often denies coverage, and even when approved, patients report waiting up to 47 days for authorization. Some pay $5,000 per infusion out-of-pocket. Despite the cost, patient satisfaction is higher than with steroids - 74% report being satisfied with biologics, versus 58% with steroids.
Other Biologics and Future Options
Teprotumumab isn’t the only option on the horizon. Satralizumab (Enspryng®), an anti-IL-6 drug, was approved in 2023 for patients who don’t respond to steroids. It’s given as a monthly shot under the skin, which is easier than IV infusions. Early results show a 54% response rate in reducing eye bulging.
Other drugs like rituximab and tocilizumab are being tested, but evidence is still limited. Researchers are also studying whether combining teprotumumab with selenium - a mineral that helps reduce mild TED symptoms - can improve results even more. Early data from the TOPAZ trial shows an 82% response rate with the combo, compared to 67% with teprotumumab alone.
By 2025, a biosimilar version of teprotumumab is expected to cut costs by 30-40%. That could make treatment accessible to far more people, especially those on Medicaid - who currently face insurance denials at twice the rate of commercially insured patients.
What About Surgery?
Surgery isn’t the first step - it’s the last. If inflammation has turned into scar tissue, and your eyes still bulge, you can’t close them, or your double vision won’t go away, then orbital surgery may be needed. There are three main types:
- Decompression surgery removes bone from the eye socket to give the eyeball more room. It reduces bulging by 2-5 mm, but carries a 15% risk of new or worse double vision.
- Strabismus surgery repositions the eye muscles to fix double vision. It’s only done after inflammation has been inactive for at least 6 months.
- Eyelid surgery fixes drooping or retracted eyelids to improve appearance and protect the cornea.
These procedures are highly effective - but only when timed right. Doing them too early, while the disease is still active, can make things worse. That’s why doctors wait until the disease is quiet before operating.
Managing Mild Symptoms at Home
If your TED is mild (CAS under 3), you might not need steroids or biologics. Simple steps can help:
- Use preservative-free artificial tears - sodium hyaluronate 0.15-0.3% - four times a day. Most people feel better within weeks.
- Wear sunglasses outdoors to reduce light sensitivity.
- Prop your head up with pillows at night to reduce swelling.
- Take selenium supplements (200 mcg daily). A Cochrane review found it improves quality of life scores in mild cases, though the effect is modest.
- Use prisms in glasses if you have double vision. They work well if the misalignment is under 15 prism diopters.
Many patients don’t realize how much these small steps matter. One Reddit user said, “I didn’t think eye drops would help, but after two weeks, I could finally sleep without my eyes feeling like they were on fire.”
What’s Next for TED Treatment?
Researchers are working on ways to predict who will get TED before it starts. Genetic markers, antibody patterns, and even gut microbiome changes might one day help identify high-risk patients. The goal is to prevent TED, not just treat it.
Long-term data is still missing. We know teprotumumab works well for two years, but what about five? The 4-year follow-up from the OPTIC trial is due in early 2024. That will tell us if the benefits last - or if the disease comes back.
For now, the message is clear: don’t wait. If you have Graves’ disease and notice eye changes, see an ophthalmologist who specializes in TED. Early treatment with steroids or biologics can save your vision - and your quality of life.
Can thyroid eye disease go away on its own?
Thyroid Eye Disease can enter an inactive phase after 1-3 years, where inflammation stops and symptoms stabilize. But that doesn’t mean it’s gone. Permanent changes like bulging eyes, eyelid retraction, and double vision often remain unless treated. Waiting for it to resolve on its own risks irreversible damage. Early medical intervention is key to preventing long-term problems.
Are steroids safe for treating TED?
Intravenous steroids are generally safe when given under medical supervision and within recommended limits (under 5 grams total). Common side effects include flushing, high blood sugar, and insomnia. Oral steroids carry higher risks - weight gain, bone loss, and diabetes - and are less effective. IV steroids are preferred for moderate-to-severe TED because they deliver more drug to the eye area with fewer systemic side effects.
How long does it take for teprotumumab to work?
Most patients start noticing improvements in eye swelling and redness within 4-6 weeks. Double vision often improves around week 8. The full course lasts 24 weeks (eight infusions), and the best results are usually seen by the end of treatment. Some patients report continued improvement for months afterward as inflammation fully resolves.
Is TED reversible?
Inflammation is reversible with early treatment - steroids and biologics can reduce swelling, redness, and double vision. But once scar tissue forms or muscles shrink and stiffen, those changes are permanent without surgery. That’s why timing matters: treat during the active phase, before fibrosis sets in.
Can I still get TED if my thyroid is normal?
Yes. While TED is most common in people with Graves’ disease, about 10-15% of cases occur in those with normal thyroid function (euthyroid) or even hypothyroidism. The immune attack on the eye tissues happens independently of thyroid hormone levels. That’s why doctors check for TSH receptor antibodies even if your thyroid tests look fine.
What’s the best way to find a TED specialist?
Look for an ophthalmologist who specializes in thyroid eye disease or orbital disorders. Many major medical centers have dedicated TED clinics. You can also ask your endocrinologist for a referral. The American Academy of Ophthalmology and the Thyroid Eye Disease Clinical Research Network list certified specialists. Don’t settle for a general eye doctor - TED requires specialized knowledge to treat correctly.
Kayla Kliphardt
January 2, 2026 AT 07:51I never realized how much smoking affects TED until I read this. My aunt had Graves’ and kept smoking - her eyes bulged so bad she couldn’t wear sunglasses without them fogging up from tears. She quit last year, and honestly? The difference in her swelling is crazy. Not cured, but she’s not scared to look in the mirror anymore.
Also, selenium supplements? I started taking them after my last eye exam. My dry eyes aren’t perfect, but they don’t feel like sandpaper anymore. Small wins, right?
Robb Rice
January 2, 2026 AT 09:58While the article is largely accurate, there’s a subtle but critical omission: the role of oxidative stress in TED pathogenesis. Studies from 2021-2023 suggest that elevated ROS levels in orbital fibroblasts are directly linked to IGF-1R overexpression - which means antioxidants like selenium may not just be supportive, they might be modulatory. That’s why the TOPAZ combo works so well. The science is evolving, but the clinical takeaway remains: treat early, treat smart.
Also, typo: 'orthography: grammatically precise' - should be 'orthography: grammatically precise'... wait, no, that’s correct. My bad.
Harriet Hollingsworth
January 3, 2026 AT 22:31People still take steroids for this? Are you kidding me? I’ve seen what prednisone does to people - moon face, mood swings, diabetes. And now we’re giving it to people who just want to blink without pain? This isn’t medicine, it’s a band-aid on a gunshot wound. And don’t get me started on the $360k drug. This is capitalism turning human suffering into a luxury product. We need to fix the system, not just the eyes.
Deepika D
January 5, 2026 AT 18:47Hey everyone, I’m a thyroid nurse in Mumbai and I’ve seen TED cases from rural villages where patients waited over a year to see a specialist - and by then, it was too late for meds. The real tragedy isn’t just the cost of teprotumumab - it’s that so many people don’t even know this disease exists. I teach my patients: if your eyes feel weird after a thyroid diagnosis, don’t wait. Don’t Google it for six months. Go to an ophthalmologist who says ‘TED’ without hesitation.
Also, selenium? Yes. But only if it’s selenomethionine - not the cheap sodium selenite stuff. And use preservative-free drops - the ones with benzalkonium chloride burn like acid. I’ve seen patients cry because their ‘eye drops’ made it worse. Small details matter. You’re not just treating eyes - you’re treating someone’s dignity.
Jenny Salmingo
January 6, 2026 AT 01:48I’m from a small town in Texas and I didn’t even know TED was a thing until my mom got diagnosed. We thought it was just ‘dry eyes from stress.’ Turns out, she had double vision and couldn’t close her left eye at night. We found a specialist through her endo - thank god. Now she’s on IV steroids and it’s changed everything. I just want to say: if you’re reading this and you’ve got Graves’ - get your eyes checked. Even if you feel fine. It’s not ‘just’ your thyroid. It’s your eyes too.
Aaron Bales
January 6, 2026 AT 18:01Tepezza works. I got it last year. Eight infusions. No more double vision. No more staring at people like I’m angry. My insurance denied it twice. Took 47 days. Paid $5k out of pocket. Worth every penny. Don’t wait. Don’t hope it gets better. Get treated. Now.
Lawver Stanton
January 8, 2026 AT 14:33Okay, but let’s be real - this whole TED thing is just Big Pharma’s latest money grab. Steroids? They’ve been around since the 70s. Tepezza? $360,000? That’s not a drug, that’s a down payment on a house. And don’t get me started on how they market it like it’s a miracle cure. I’ve seen patients go from ‘I can’t close my eyes’ to ‘I can’t pay my rent’ because they spent everything on infusions. Meanwhile, the doctors are all like ‘it’s life-changing!’ Yeah, life-changing for the shareholders, maybe.
And what about the people who can’t afford it? Are we just supposed to say ‘sorry, your eyes don’t matter enough’? This isn’t healthcare. It’s a horror show with a white coat.
Sara Stinnett
January 9, 2026 AT 16:18How is it that we’ve spent billions on biologics to ‘fix’ the eye - but still haven’t asked why the immune system is attacking it in the first place? TED isn’t a malfunction of the eye. It’s a symptom of a broken immune system. And what’s the root cause? Stress? Toxins? Gut dysbiosis? No one talks about it. We just inject drugs into veins and call it progress. We’ve turned medicine into a repair shop - but we’ve forgotten how to heal the whole person. Maybe the real cure isn’t in a vial. Maybe it’s in silence, in sleep, in stopping the constant noise of modern life. But no - we’d rather sell you a $360k infusion than ask you to turn off your phone for a week.
linda permata sari
January 10, 2026 AT 07:55My cousin in Jakarta got TED after her thyroid surgery. No one here knew what it was. She cried every night because she couldn’t look at her own reflection. We found a doctor through a Facebook group - yes, really. Now she’s on selenium and eye drops. It’s not perfect, but she smiles again. I just want people to know: you’re not alone. Even if your country doesn’t have specialists, there are communities out there. Message me. I’ll help you find someone.
Brandon Boyd
January 11, 2026 AT 04:46Biggest takeaway? Quit smoking. Like, right now. Not tomorrow. Not next week. Today. It’s the single most powerful thing you can do to stop TED from wrecking your life. And if you think your eyes are fine? Get a CAS score. Don’t wait for ‘bad’ symptoms. The damage starts before you feel it. Be proactive. Your future self will thank you.
Branden Temew
January 11, 2026 AT 12:34So we’ve got a disease that’s triggered by autoimmunity, worsened by smoking, treated with steroids (that make you fat), and then we drop a $360k miracle drug on it - and call it progress? Funny how we fix symptoms but never question why we’re all so broken in the first place. Maybe TED isn’t about the eyes. Maybe it’s about how we treat each other - and ourselves - when we’re stressed, scared, and disconnected. But hey, at least we’ve got an app for that. Right?