Warfarin Diet Guide: Keep Vitamin K Foods Consistent for Stable INR
Learn how to keep your warfarin therapy stable by eating consistent amounts of vitamin K foods, tracking meals, and working with your healthcare team.
Read MoreWhen managing INR stability, the consistency of International Normalized Ratio values while on blood‑thinning therapy, you’re juggling several moving parts. One core player is warfarin, a vitamin K antagonist that slows clot formation. Another essential factor is Vitamin K, a dietary nutrient that directly opposes warfarin’s effect. Both of these entities influence the third key element—a anticoagulation clinic, a health‑care setting that provides regular INR testing and dose adjustments. Together they form the backbone of any strategy that wants to keep INR numbers steady.
Patients who achieve INR stability reduce their risk of both dangerous clots and bleeding events. The target range—usually 2.0 to 3.0 for most conditions—acts like a sweet spot. Drop below and you risk a thrombus; rise above and bleeding becomes a real threat. This balance is not static; it reacts to changes in diet, other medicines, and even infections. For instance, a sudden increase in leafy greens floods the system with Vitamin K, which can push the INR down. Conversely, taking antibiotics that kill gut bacteria can raise the INR unexpectedly. Understanding these cause‑and‑effect relationships is the first step toward mastering stable results.
Beyond food, drug interactions play a massive role. DOACs, direct oral anticoagulants that work without routine INR checks are often mentioned as alternatives when stability proves hard to maintain. However, many patients stay on warfarin because of cost, specific medical indications, or physician preference. When warfarin remains the choice, the anticoagulation clinic steps in to fine‑tune doses based on trends, not single readings. This ongoing monitoring creates a feedback loop: regular testing informs dose changes, which in turn influence future INR values, reinforcing stability over time.
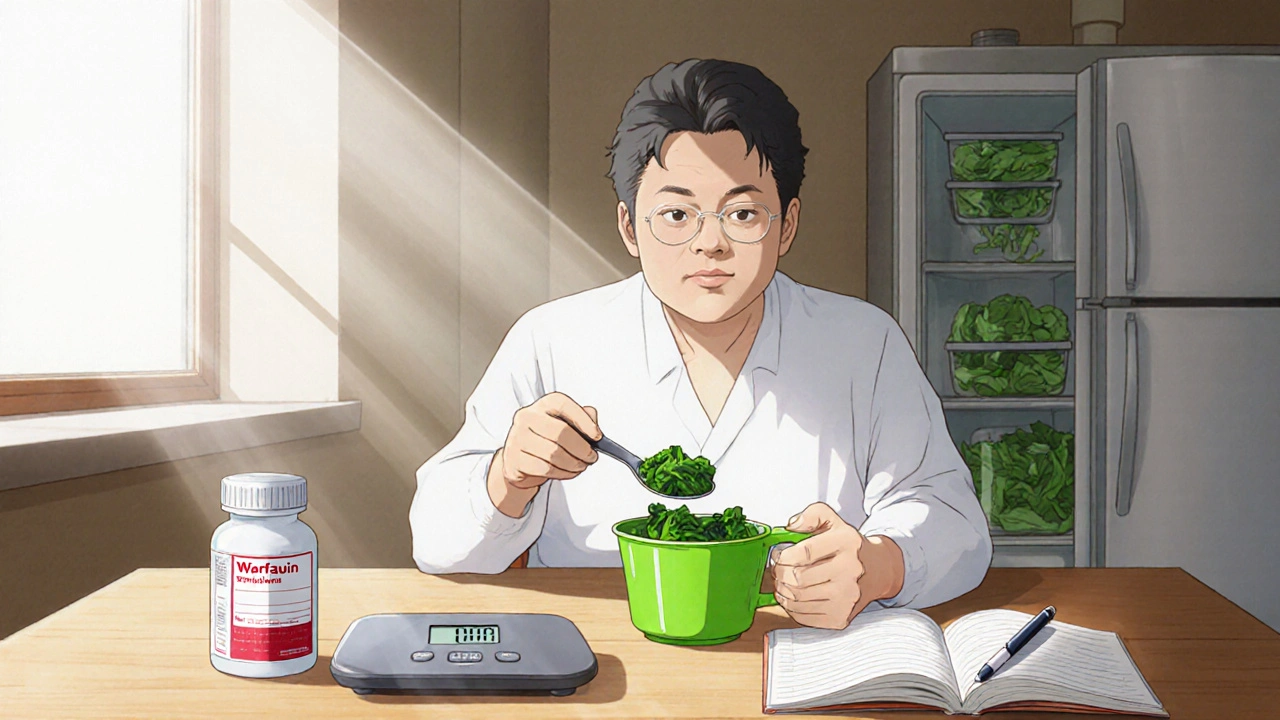
Practical steps to boost INR stability start with a predictable diet. Aim for a steady amount of Vitamin K each day—think about keeping your spinach, kale, and broccoli servings consistent rather than swinging from zero to a huge plate. Keep a medication list handy and share it with your clinic; even over‑the‑counter drugs like ibuprofen can tip the balance. If you’re ill, especially with fever or a gastrointestinal infection, let the clinic know right away—they may adjust the warfarin dose temporarily. Finally, commit to the testing schedule your anticoagulation clinic sets. Skipping a test can hide a trend until it becomes dangerous.
All of these pieces—warfarin dosing, Vitamin K intake, clinic‑driven monitoring, and awareness of other drugs like DOACs—interlock to create a stable INR environment. Below you’ll find articles that dig deeper into each of these factors, from the science behind warfarin metabolism to real‑world tips for diet management. Browse the collection to discover how you can turn the abstract goal of "INR stability" into a daily routine that keeps you safe and confident on your anticoagulant therapy.
Learn how to keep your warfarin therapy stable by eating consistent amounts of vitamin K foods, tracking meals, and working with your healthcare team.
Read More