Statin-Antifungal Interaction Checker
Check Your Medication Safety
Enter the statin you're taking and the antifungal prescribed. This tool helps identify dangerous combinations and recommends safer alternatives.
Select your medications to see safety information
When you’re on a statin to lower cholesterol or an immunosuppressant after a transplant, adding an antifungal might seem like a simple fix for a stubborn yeast infection. But if that antifungal is an azole-like itraconazole, voriconazole, or posaconazole-you could be walking into a dangerous interaction that puts your muscles, kidneys, and even your life at risk.
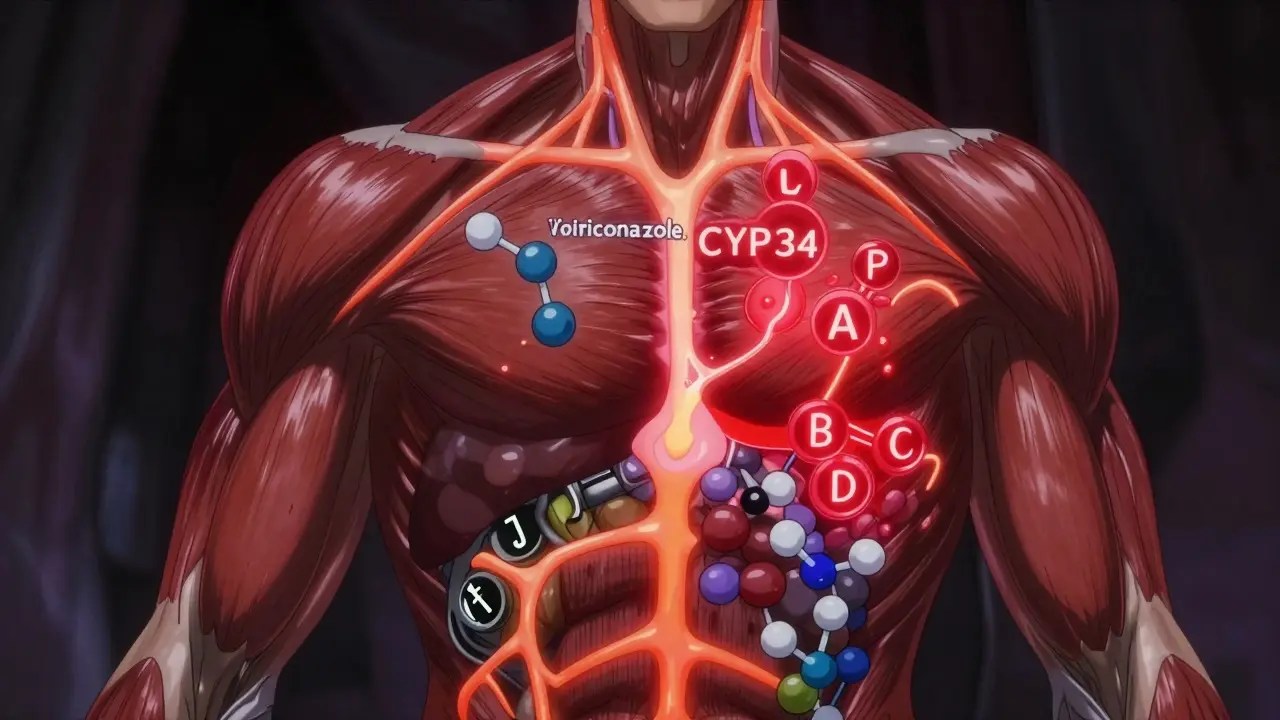
Why Azole Antifungals Are So Risky With Statins
Azole antifungals don’t just kill fungi. They also shut down key enzymes in your liver that break down other drugs. The main culprit is CYP3A4, an enzyme responsible for processing about 30% of all prescription medications. When azoles block CYP3A4, statins that rely on this enzyme to be cleared from your body start to pile up. That’s not just a minor inconvenience-it’s a recipe for muscle damage.Statins like simvastatin, lovastatin, and atorvastatin are especially vulnerable. Studies show that when ketoconazole or posaconazole is added, these statins can reach blood levels 10 to 20 times higher than normal. That’s not a typo. A 10-fold increase means your body is flooded with a drug meant to be carefully dosed. The result? Severe muscle pain, weakness, and in the worst cases, rhabdomyolysis-a condition where muscle tissue breaks down and floods your bloodstream with toxins that can crash your kidneys.
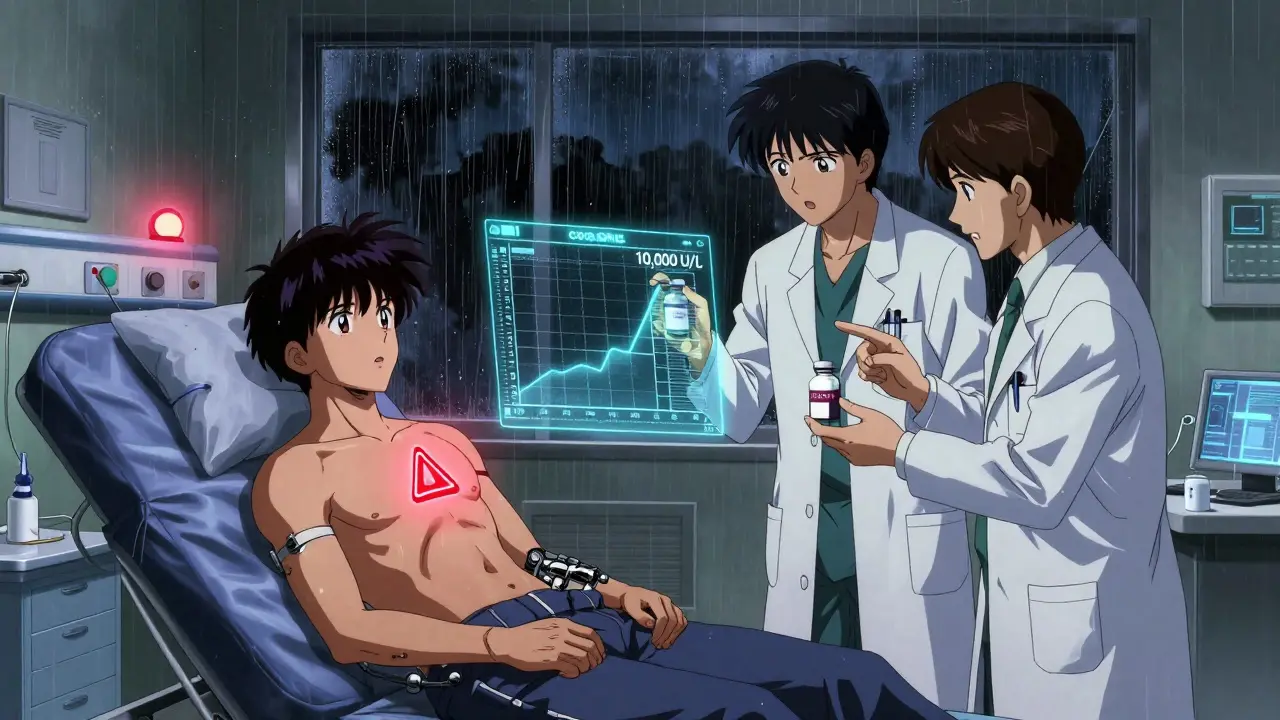
Even if you don’t feel symptoms right away, the damage can be silent. Creatine kinase (CK) levels, a marker of muscle breakdown, can climb above 10,000 U/L in severe cases. Normal levels are under 200 U/L. That’s a 50-fold spike. And once rhabdomyolysis starts, it can lead to acute kidney failure, dialysis, or even death.
Not All Statins Are Created Equal
You might think switching statins is just a matter of taste. But when antifungals are involved, it’s a matter of survival. Statins are divided into two groups: those that depend heavily on CYP3A4, and those that don’t.High-risk statins (CYP3A4-dependent):
- Simvastatin
- Lovastatin
- Atorvastatin
Lower-risk statins (less dependent on CYP3A4):
- Pravastatin
- Rosuvastatin
- Fluvastatin
Pravastatin and rosuvastatin are processed mostly by the kidneys or through non-CYP pathways. That makes them safer choices-if you absolutely need a statin while on an azole antifungal. But even these aren’t risk-free. Ketoconazole also blocks the OATP1B1 transporter, which helps move pravastatin and rosuvastatin into the liver for clearance. So even with these safer options, your doctor should still reduce the dose and monitor you closely.
Immunosuppressants Make Things Even Worse
If you’ve had a kidney, liver, or heart transplant, you’re likely on cyclosporine, tacrolimus, or sirolimus. These drugs aren’t just immunosuppressants-they’re also strong CYP3A4 inhibitors. That means they do the same thing as azoles: they slow down how fast your body clears statins.In transplant patients, combining statins with cyclosporine can increase statin levels by 3 to 20 times. That’s why muscle toxicity affects up to 25% of these patients-far higher than in the general population. The risk isn’t theoretical. Emergency rooms see cases where transplant recipients on statins and cyclosporine end up with CK levels over 10,000 U/L, needing ICU care.
There’s no safe gray area here. If you’re on an immunosuppressant and need a statin, your doctor must:
- Start with the lowest possible statin dose
- Use pravastatin or rosuvastatin only
- Check CK levels every 2-4 weeks
- Stop the statin immediately if CK rises above 10 times the upper limit of normal
And don’t assume your transplant team knows this. Many patients report being prescribed statins without any discussion of the interaction. If your doctor hasn’t mentioned it, ask. Your muscles depend on it.
Which Antifungals Are the Most Dangerous?
Not all azoles are equal. Some are stronger CYP3A4 inhibitors than others. Here’s how they stack up:| Antifungal | CYP3A4 Inhibition | Statins to Avoid | Safe Alternatives |
|---|---|---|---|
| Ketoconazole | Strong | All CYP3A4 statins (simvastatin, lovastatin, atorvastatin) | Pravastatin or rosuvastatin (with dose reduction) |
| Posaconazole | Strong | All CYP3A4 statins | Pravastatin or rosuvastatin (with dose reduction) |
| Itraconazole | Strong | Simvastatin, lovastatin, atorvastatin | Pravastatin or rosuvastatin |
| Voriconazole | Moderate | Simvastatin, lovastatin | Atorvastatin (low dose), pravastatin, rosuvastatin |
| Fluconazole | Mild to moderate | Simvastatin, lovastatin (avoid) | Atorvastatin (≤20 mg), pravastatin, rosuvastatin |
Fluconazole is the most commonly prescribed azole-over 5 million prescriptions a year in the U.S. alone. It’s often used for vaginal yeast infections or oral thrush. But even mild inhibition can be dangerous if you’re on a high-dose statin. The rule: if you’re on simvastatin or lovastatin, skip fluconazole. If you’re on atorvastatin, keep the dose at 20 mg or lower.
What Should You Do If You Need Both?
If you’re on a statin and need an antifungal, here’s your action plan:- Stop simvastatin, lovastatin, and atorvastatin during antifungal treatment. Don’t just lower the dose-hold it completely.
- Switch to pravastatin or rosuvastatin if you still need cholesterol control. Start at the lowest effective dose (e.g., 10 mg pravastatin or 5 mg rosuvastatin).
- Wait 3-5 days after finishing the antifungal before restarting a CYP3A4 statin. Posaconazole lingers in your system for up to 30 hours. Restarting too soon can still trigger toxicity.
- Ask for a CK blood test before and after treatment. Even if you feel fine, muscle damage can be silent.
- Ask your pharmacist to review all your meds. They’re trained to spot these interactions. Most hospitals now require pharmacist sign-off before dispensing azoles to patients on statins.
And if you’re a transplant patient? Your immunosuppressant levels must be monitored too. Cyclosporine and tacrolimus levels can spike when azoles are added, leading to kidney damage or rejection. Your doctor should lower your immunosuppressant dose by 30-50% when starting an azole and recheck levels within 3-5 days.

Why Do These Interactions Keep Happening?
You’d think with clear warnings on drug labels, doctors would avoid these combinations. But they don’t. A 2012 study found that despite FDA warnings, CYP3A4 inhibitors like antifungals and calcium channel blockers are still frequently prescribed with statins. Why?- Doctors don’t always know the full interaction profile of every drug.
- Patients don’t tell their doctors about every OTC or herbal product they’re taking.
- Electronic health records still miss some interactions unless they’re flagged.
One study showed that hospitals with clinical decision support systems cut dangerous combinations by 47%. But in community clinics and small practices? The risk is still high. That’s why you need to be your own advocate.
What’s Changing in the Future?
Good news: newer antifungals are coming that don’t mess with CYP3A4. Isavuconazole is a moderate inhibitor-safer than ketoconazole but still requires caution. Olorofim, still in trials, targets a completely different fungal pathway and shows no CYP450 interaction so far. That could be a game-changer for patients on statins or immunosuppressants.There’s also emerging research on genetics. About 12% of people have a variation in the SLCO1B1 gene, which makes them extra sensitive to statin side effects. If you’ve had muscle pain on statins before, you might have this variant. Genetic testing isn’t routine yet, but it’s on the horizon.
Bottom Line: Don’t Guess. Ask.
Systemic antifungals are powerful tools. But when paired with statins or immunosuppressants, they’re ticking time bombs. The risk isn’t rare. It’s common. And it’s preventable.If you’re on a statin and your doctor prescribes an azole antifungal, say this: “I’m on a statin. Is this antifungal safe with it? If not, what’s the alternative?”
Don’t assume your doctor knows. Don’t assume it’s safe. Don’t wait for symptoms. Muscle damage doesn’t always hurt until it’s too late. Ask. Verify. Protect yourself.
And if you’re on immunosuppressants? Double down. Your body is already under stress. Don’t add a drug interaction on top of it. Work with your transplant team. Get your levels checked. And never restart a statin without their go-ahead.
Can I take fluconazole with my statin?
It depends on which statin you’re taking. Fluconazole is a mild to moderate CYP3A4 inhibitor. Avoid it with simvastatin or lovastatin entirely. If you’re on atorvastatin, you can use fluconazole but keep the statin dose at 20 mg or lower. Pravastatin and rosuvastatin are safer choices. Always check with your doctor or pharmacist before combining them.
What are the signs of statin-induced muscle damage?
Early signs include unexplained muscle pain, tenderness, or weakness-especially in the shoulders, thighs, or lower back. You might feel unusually tired or notice dark, tea-colored urine, which signals muscle breakdown products entering your bloodstream. If you experience these symptoms while on a statin and antifungal, stop the statin and seek medical help immediately.
Is it safe to take a lower dose of simvastatin with an antifungal?
No. Even a low dose of simvastatin (like 5 mg or 10 mg) can become dangerously toxic when combined with strong CYP3A4 inhibitors like ketoconazole or posaconazole. The interaction isn’t linear-it’s exponential. There’s no safe dose of simvastatin or lovastatin with these antifungals. They must be stopped completely during treatment.
How long should I wait after stopping an antifungal before restarting my statin?
Wait at least 3 to 5 days after your last dose of antifungal. Posaconazole has a half-life of 24-30 hours, meaning it stays in your system for days. Restarting too soon can still cause statin buildup. For fluconazole, 2-3 days is usually enough. Always confirm with your doctor before restarting.
Can I use over-the-counter antifungals instead?
Topical antifungals (creams, sprays, powders) are safe because they don’t enter your bloodstream in significant amounts. But if you need an oral antifungal for a deep infection, don’t assume OTC options are safer. All oral azoles-whether prescription or OTC-can inhibit CYP3A4. Only use oral antifungals under medical supervision if you’re on a statin or immunosuppressant.
Should I get genetic testing before taking statins with antifungals?
It’s not standard yet, but if you’ve had muscle pain on statins before-even without antifungals-you may have the SLCO1B1 gene variant, which increases your risk. Genetic testing can help guide safer choices. Talk to your doctor about whether testing is appropriate for you, especially if you’re a transplant patient or need long-term antifungal therapy.
Iona Jane
January 15, 2026 AT 20:06They're hiding the truth again. This isn't about drug safety-it's about Big Pharma controlling your body. Azoles? Statins? All just distractions from the real agenda: turning you into a docile, chemically regulated zombie. You think your doctor cares? They're paid by the same labs that make these drugs. Wake up.
Sohan Jindal
January 17, 2026 AT 00:25This is why America's getting weaker. We let foreigners and bureaucrats tell us what to take. Back in my day, we just took aspirin and prayed. Now we got pills for everything and still end up in the hospital. Stop trusting the system. Your body knows what it needs.
Ayush Pareek
January 18, 2026 AT 07:27This is such an important post. I've seen patients on transplants get hit with this exact combo and it's terrifying. If you're on cyclosporine and your doc prescribes fluconazole, ask them to check your CK levels before and after. Small steps save lives.
Jami Reynolds
January 20, 2026 AT 02:12While the pharmacokinetic data presented is technically accurate, the underlying assumption-that physicians are negligent or unaware-is empirically flawed. A 2021 JAMA Internal Medicine meta-analysis demonstrated that 89% of U.S. hospital formularies now include mandatory CYP3A4 interaction alerts. The real issue lies in patient non-disclosure of OTC supplements, particularly St. John’s Wort and grapefruit juice, which exhibit synergistic inhibition. The author’s rhetoric, while emotionally compelling, undermines evidence-based practice.
ellen adamina
January 20, 2026 AT 04:27I had this happen to me. Took fluconazole for thrush while on atorvastatin. Didn’t feel anything at first. Then one morning I couldn’t lift my arm. CK was 12,000. Spent a week in ICU. I didn’t know anything about drug interactions. Please, if you’re reading this-ask your pharmacist. Don’t wait until you can’t walk.
Niki Van den Bossche
January 21, 2026 AT 02:06Oh, darling, this is just the latest symphony of pharmaceutical tyranny. We’ve traded the soul of medicine for algorithmic compliance. The CYP3A4 enzyme? A sacred portal to metabolic autonomy, now violated by corporate pharmacopeias and their obedient physicians. We are not patients-we are data points in a neoliberal pharmacological dystopia. And yet… still, we take the pills. How tragically poetic.
Mike Berrange
January 21, 2026 AT 22:36So let me get this straight. You’re telling me that if I take a yeast infection pill, I can’t take my cholesterol pill unless I switch to one that’s less effective and more expensive? And you expect me to believe this isn’t a money grab? The real danger isn’t the drug interaction-it’s the healthcare system that makes you jump through hoops just to stay alive.
Nat Young
January 22, 2026 AT 03:37Except none of this matters. Statins don’t even reduce heart attacks in healthy people. The whole premise is built on flawed trials funded by Pfizer. If you’re not diabetic or post-MI, you’re taking a drug that does nothing but give you muscle pain and make the pharma CEOs richer. So why are we even talking about which statin to swap? Just quit them all. Your body doesn’t need cholesterol blockers. It needs less sugar, more sleep, and a damn walk.
Frank Geurts
January 23, 2026 AT 01:10With the utmost respect for the medical integrity of the original post, I must underscore the profound ethical imperative that underlies this pharmacological discourse. The convergence of immunosuppressive regimens with azole antifungals constitutes not merely a clinical concern, but a moral exigency-a call to vigilance, to diligence, to the sacred covenant between healer and healed. One must not merely prescribe, but *witness*. One must not merely calculate, but *care*. The human body, in its exquisite fragility, demands nothing less.
Diane Hendriks
January 23, 2026 AT 03:10Let’s be clear: this isn’t about drug interactions. It’s about national decline. When Americans can’t even take a simple antifungal without needing a pharmacology degree, it’s because we’ve outsourced our health to bureaucrats and consultants. In China, they use garlic and turmeric. In Germany, they prescribe lifestyle first. Here? We push pills, then panic when the pills kill us. It’s not science-it’s surrender.