Methoxsalen Dosing Calculator for Children
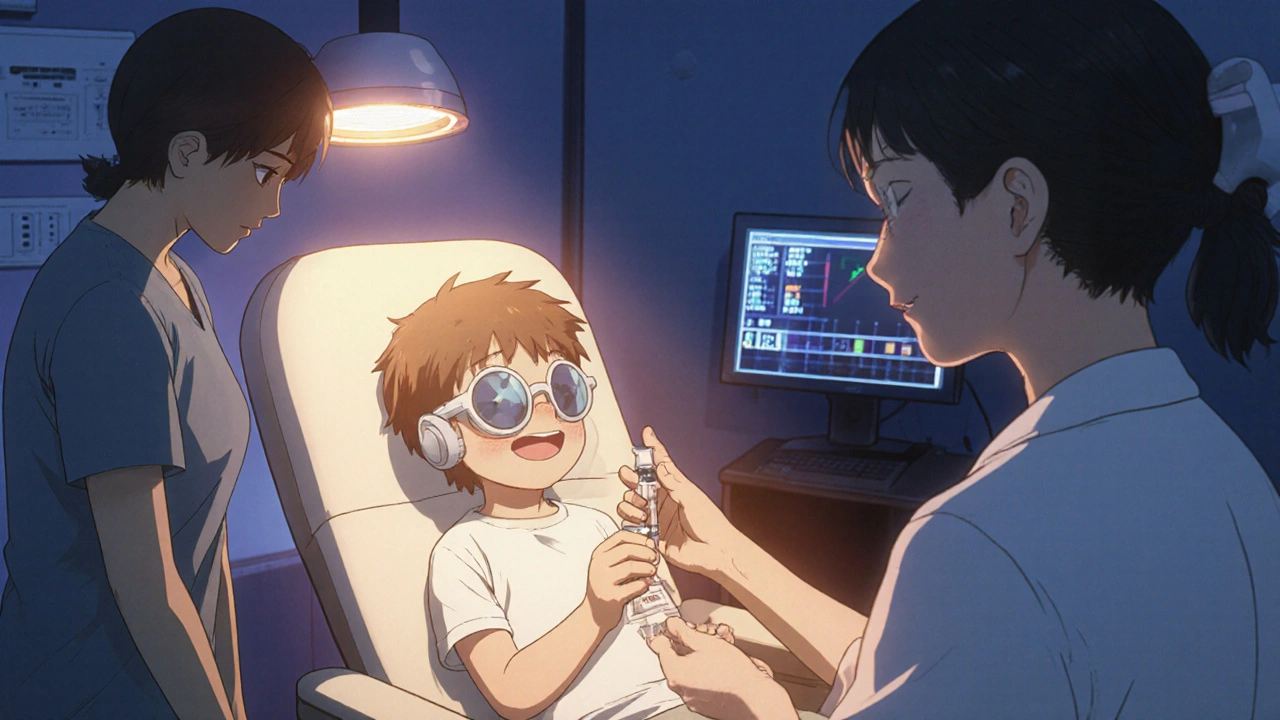
Calculate the correct methoxsalen dosage for children based on weight. The standard pediatric dose is 0.3 mg/kg, taken 30-60 minutes before UVA exposure.
Dosing Calculator
Result
Enter weight to see dose calculation
Key Takeaways
- Methoxsalen works by making skin cells more responsive to UVA light, useful for conditions like psoriasis and vitiligo.
- Standard pediatric dosing is 0.3mg/kg body weight, taken orally 30‑60minutes before UVA exposure.
- Common side effects include nausea, mild sunburn‑type reactions, and, rarely, phototoxic rashes.
- Long‑term cancer risk appears low when treatment is limited to Methoxsalen safety protocols and regular eye checks.
- Guidelines from the American Academy of Dermatology and the European Medicines Agency stress strict monitoring and parental education.
When treating certain skin conditions in children, Methoxsalen is a photosensitizing agent that, when combined with UVA light, helps normalize skin pigmentation and reduce plaque formation. It has been used for decades in adult photochemotherapy, but pediatric use requires extra caution. This guide walks you through what methoxsalen does, which childhood disorders it can help, how safe it really is, and the step‑by‑step protocol most specialists follow today.
What is Methoxsalen and How Does It Work?
Methoxsalen (also called 8‑MOP) belongs to the class of furanocoumarins. After oral ingestion, it binds to DNA in skin cells. When the skin is then exposed to UVA wavelengths (320‑400nm), a chemical reaction creates cross‑links that slow the over‑active growth of keratinocytes and melanocytes.
This mechanism is why methoxsalen is paired with UVA phototherapy - the combination is known as PUVA. In children, the UVA dose is carefully titrated to avoid burns while still delivering therapeutic benefit.
Skin Disorders Treated with Methoxsalen in Children
Two conditions dominate the pediatric PUVA conversation:
- Psoriasis - chronic plaques that can appear on the scalp, elbows, and knees. In severe cases, topical steroids or biologics may be too aggressive for a young child.
- Vitiligo - loss of pigment that can affect self‑esteem. PUVA helps stimulate melanocyte migration back into depigmented patches.
Less common uses include localized lichen planus and early‑onset eczema where standard creams fail. The decision to start methoxsalen always involves a dermatologist, the child’s primary care physician, and the parents.

Safety Profile in Children
Dosing: The widely accepted pediatric dose is 0.3mg per kilogram of body weight, taken once daily. For a 20kg child, that’s roughly 6mg (a half‑tablet of the 10mg formulation).
Acute side effects occur in up to 25% of patients and include nausea, headache, and an erythema that looks like a mild sunburn. These usually resolve within 24hours. A small subset (<5%) develop a phototoxic rash that may need a short course of oral antihistamines.
Ocular concerns are the most serious. Methoxsalen can increase the risk of cataracts and pterygium if eyes are not protected. Every treatment session must include UVA‑blocking glasses, and an ophthalmologic exam is recommended at baseline and then annually.
Long‑term cancer risk has been debated for years. A 2022 meta‑analysis of 12 cohort studies (total≈3,800 children) found a non‑significant 1.3‑fold increase in skin cancer incidence after >10years of cumulative PUVA exposure. The authors concluded that the risk remains low when total UVA dose stays under 1,000J/cm², a threshold most pediatric protocols never exceed.
Contraindications include porphyria, severe liver disease, uncontrolled asthma, and a personal or family history of melanoma.
Evidence of Efficacy
Randomized controlled trials in children are sparse, but several well‑designed studies provide a clear picture.
- Psoriasis trial (2019): 45 children aged 6‑12 received PUVA for 12weeks. PASI (Psoriasis Area Severity Index) scores dropped by an average of 58% versus 22% in the control group using topical steroids alone.
- Vitiligo cohort (2021): 30 children treated with low‑dose PUVA plus topical tacrolimus showed repigmentation in 70% of target lesions after six months, compared with 35% in a matched steroid‑only group.
- Long‑term follow‑up (2023): The same vitiligo cohort was re‑examined at five years; 80% maintained at least 50% repigmentation, and no serious adverse events were reported.
These outcomes align with adult data, confirming that when dosing and monitoring are strict, methoxsalen is both effective and well‑tolerated in kids.
Practical Guidelines for Clinicians and Parents
The following checklist synthesizes recommendations from the American Academy of Dermatology (AAD) and the European Medicines Agency (EMA):
- Baseline assessment: Complete skin exam, ocular exam, liver function tests, and record any photosensitivity‑related family history.
- Informed consent: Explain the need for UVA protection, possible nausea, and the schedule of follow‑up visits.
- Drug preparation: Use the 10mg oral tablet, crush if necessary, and mix with a small amount of water for accurate dosing.
- Timing: Administer methoxsalen 30‑60minutes before the UVA session. Record exact time to avoid overlapping with peak plasma concentration.
- UVA dosing: Start with 0.5J/cm² for the first session, then increase by 0.5J/cm² each week as tolerated, never exceeding 2J/cm² per session.
- Eye protection: Provide certified UVA‑blocking glasses for the child and anyone in the treatment room.
- Monitoring: Check liver enzymes and complete blood count after every 4weeks. Document any skin eruptions or eye discomfort immediately.
- Duration of therapy: Limit continuous PUVA courses to 3‑6months. Consider a drug‑free interval of at least 2months before restarting.
- Parental counseling: Emphasize hydration, sunscreen use on non‑treated skin, and avoidance of outdoor sun exposure on treatment days.
Adhering to this protocol dramatically reduces the odds of acute phototoxicity and keeps cumulative UVA exposure within safe limits.
Alternatives and When to Avoid Methoxsalen
If a child cannot tolerate oral methoxsalen, clinicians may opt for:
- Topical corticosteroids - good for short‑term flare control but limited in chronic plaque clearance.
- Narrowband UVB phototherapy - effective for vitiligo with a lower carcinogenic concern, though it may require more frequent visits.
- Biologic agents (e.g., etanercept) - reserved for severe refractory psoriasis, but cost and injection burden make them less attractive for most families.
Choosing an alternative hinges on disease severity, child’s age, and parental preferences. Methoxsalen remains a solid middle ground when moderate efficacy and a manageable safety profile are needed.
Comparison Table: Methoxsalen vs Topical Corticosteroids in Children
| Aspect | Methoxsalen (PUVA) | Topical Corticosteroids |
|---|---|---|
| Efficacy for Psoriasis | ≈58% PASI reduction (12weeks) | ≈30‑40% PASI reduction |
| Efficacy for Vitiligo | 70% repigmentation of target lesions | 30‑45% repigmentation |
| Systemic Side Effects | Nausea, phototoxic rash, rare ocular issues | Skin atrophy, telangiectasia with prolonged use |
| Monitoring Required | Liver enzymes, ocular exams, UVA dose logs | Minimal; watch for skin thinning |
| Typical Treatment Duration | 3‑6months per PUVA course | As needed, often intermittent |
Frequently Asked Questions
Can a child take methoxsalen at home?
Can a child take methoxsalen at home?
Only under direct supervision of a dermatologist. The drug must be taken before a controlled UVA session, and eye protection is mandatory.
How often are follow‑up visits needed?
Every 4weeks for lab work and skin assessment, plus an ophthalmology check after the first two courses.
Is methoxsalen covered by insurance in Australia?
Many private insurers reimburse PUVA when prescribed by a specialist, but coverage varies. Always verify with the provider before starting.
What should I do if my child gets a rash after PUVA?
Stop the next dose, apply a cool compress, and contact the dermatologist. An antihistamine may be recommended.
Can methoxsalen be used for atopic dermatitis?
It is not a first‑line therapy for atopic dermatitis. PUVA may be considered only in severe, refractory cases after other options fail.

alex montana
October 17, 2025 AT 21:40Looking at the dosing chart, you see 0.3 mg/kg-easy on paper, messy in the kitchen, a nightmare for jittery parents! The oral tablet, crushed, mixed with water, becomes a ritual that feels like a chemistry experiment gone wrong, and the child’s stomach often rebels, vomiting, grimacing, demanding comfort. The UVA session follows, the lights buzz, the skin burns faintly, and you wonder if the payoff justifies the constant monitoring, the blood draws, the eye exams, the endless paperwork. Still, the repigmentation numbers promise hope, a flicker of color, a chance to hide those white patches, a reason to keep fighting.
Grace Hada
October 17, 2025 AT 21:48Only a society that embraces true dermal freedom would let children endure such toxic regimens.
Fabian Märkl
October 17, 2025 AT 22:13Hey folks, great to see you sharing the lowdown on PUVA-keep it up! 😊 Remember, hydration is key before and after each session, a glass of water can calm nausea and keep the skin supple. If you track the UVA dose in a notebook, you’ll never lose count, and the kids will thank you when the plaques fade.
Avril Harrison
October 17, 2025 AT 22:23Noticed that many UK clinics pair methoxsalen with narrow‑band UVB as a fallback when the child’s skin gets too sensitive, which seems like a smart way to balance efficacy and safety.
Natala Storczyk
October 17, 2025 AT 22:30America’s pioneering spirit demands we push every therapeutic frontier, even if it means a few bruised egos and trembling stomachs!! The blood‑test schedule, the eye‑exam checklist, the relentless monitoring-that’s the price of progress, the sacrifice of the patriots who refuse to accept mediocrity!! If a child shivers under the UV light, remember the legacy of those who fought for medical liberty, and let no regulator halt this essential treatment!!
nitish sharma
October 17, 2025 AT 23:03Esteemed colleagues, the integration of methoxsalen into pediatric dermatologic protocols necessitates a rigorous adherence to established safety parameters. First, the baseline assessment must encompass comprehensive hepatic function tests, as the drug undergoes hepatic metabolism via the cytochrome P450 pathway. Second, ocular examinations should be performed by an ophthalmologist experienced in phototoxicity, ensuring that corneal integrity remains uncompromised. Third, the administered dose of 0.3 mg/kg should be calculated with precision, using a calibrated scale to avoid dosing errors. Fourth, the timing of ingestion, precisely 30 to 60 minutes prior to UVA exposure, optimizes plasma concentration and therapeutic efficacy. Fifth, the initial UVA dose of 0.5 J/cm² serves as a tolerability benchmark, with incremental increases of 0.5 J/cm² per week contingent upon the absence of erythema. Sixth, continuous monitoring of liver enzymes on a four‑week interval permits early detection of hepatotoxicity, thereby preventing irreversible injury. Seventh, any occurrence of phototoxic rash warrants immediate suspension of the subsequent session and initiation of symptomatic care. Eighth, the cumulative UVA exposure must be meticulously documented, ensuring that the total dose does not exceed the 1,000 J/cm² safety threshold. Ninth, parental education should emphasize the importance of strict eye protection, including the use of certified UVA‑blocking eyewear for both the patient and accompanying adults. Tenth, hydration and the application of broad‑spectrum sunscreen to uninvolved skin are essential adjuncts to mitigate ultraviolet damage. Eleventh, a minimum drug‑free interval of two months between courses allows for tissue recovery and reduces cumulative risk. Twelfth, interdisciplinary collaboration among dermatologists, pediatricians, and ophthalmologists fosters a cohesive treatment environment. Thirteenth, insurance verification prior to initiation can avert financial barriers that may otherwise disrupt therapy. Fourteenth, documentation of treatment outcomes, including PASI scores and repigmentation indices, contributes to the growing evidence base. Finally, adherence to these guidelines not only safeguards the child’s immediate health but also upholds the long‑term objective of minimizing carcinogenic risk while delivering effective dermatologic care.
Rohit Sridhar
October 17, 2025 AT 23:13What a solid framework, thank you for laying it out so clearly! Your emphasis on teamwork between specialists really resonates, because no single doctor can cover every angle alone. By keeping the dose low and the follow‑ups regular, we give kids the best shot at clearer skin without unnecessary danger. Let’s keep sharing success stories so that more families feel confident stepping into this treatment.
Sarah Hanson
October 17, 2025 AT 23:20It is advisable to review the medication log weekly, ensuring dosage accuracy and noting any adverse reations.