More than 100,000 people in the U.S. will be diagnosed with invasive melanoma this year. That’s more than double the number from 20 years ago. But here’s the thing: if caught early, your chance of surviving is over 99%. If it spreads? That number drops to 35%. The difference isn’t luck. It’s knowing what to look for, when to act, and how to protect yourself.
What Melanoma Really Is
Melanoma starts in melanocytes - the cells that give your skin its color. It’s not the most common skin cancer, but it’s the deadliest. About 1 in 50 people in the U.S. will get it in their lifetime. And unlike basal cell or squamous cell cancers, melanoma can spread fast - sometimes in weeks.
There are four main types:
- Superficial spreading melanoma - makes up 70% of cases. It grows sideways along the top layer of skin before going deeper. Often shows up as a new or changing mole.
- Nodular melanoma - 15-30% of cases. Grows quickly downward. Looks like a raised bump, often black or dark red. Can appear where no mole existed before.
- Lentigo maligna melanoma - 10-15%. Usually on sun-exposed areas like the face or arms in older adults. Starts as a flat, irregularly shaped patch.
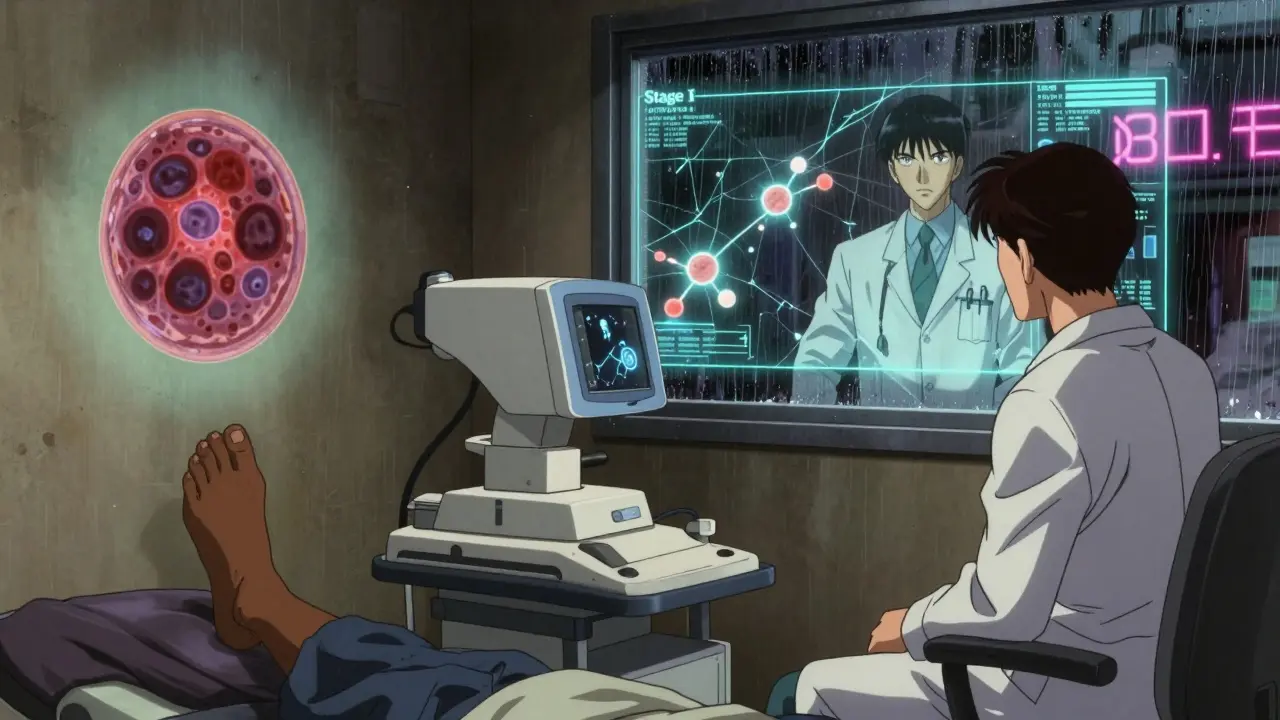
- Acral lentiginous melanoma - 2-8%. Most common in people with darker skin. Appears on palms, soles, or under nails. Often missed because it doesn’t look like a typical sun-related mole.
Half of all melanomas have a BRAF gene mutation. That’s important because it opens up targeted treatment options. But even if you don’t have that mutation, new immunotherapies are still working.
How to Prevent Melanoma
Ninety percent of melanomas are caused by UV radiation - from the sun or indoor tanning. That means most cases are preventable. But prevention isn’t just about sunscreen.
Here’s what actually works:
- Avoid tanning beds completely. People who use them before age 35 raise their melanoma risk by 58%. That’s not a small number. It’s a red flag.
- Wear broad-spectrum SPF 30+ every day. Even in winter. Even if it’s cloudy. UV rays penetrate clouds. And UVA rays - the ones that age your skin and damage DNA - are present all day, every day.
- Seek shade between 10 a.m. and 4 p.m. That’s when UV rays are strongest. Don’t wait until you’re burning to get out of the sun.
- Wear protective clothing. Hats with wide brims, UV-blocking sunglasses, long sleeves. A regular white t-shirt only blocks about 50% of UV rays. Special sun-protective fabrics with UPF 50+ block over 98%.
- Teach kids early. Skin damage from childhood builds up over time. The CDC found only 14% of high schoolers use sunscreen regularly. That needs to change.
There’s a myth that darker skin tones are immune. They’re not. Acral melanoma doesn’t care about your skin color. It shows up on the soles of feet, under nails, or between toes. And it’s often diagnosed late because people - and doctors - don’t look there.
How to Detect Melanoma Early
Early detection saves lives. The ABCDE rule is the gold standard - and it’s simple enough for anyone to use.
- A - Asymmetry: One half doesn’t match the other.
- B - Border: Edges are ragged, blurred, or notched.
- C - Color: Multiple shades of brown, black, red, white, or blue.
- D - Diameter: Larger than 6mm - about the size of a pencil eraser.
- E - Evolving: Changing in size, shape, color, or texture. Or it starts to itch, bleed, or crust.
But ABCDE isn’t enough on its own. You need to know your skin. Do a full-body self-check once a month. Take 10-15 minutes after a shower. Use a mirror. Check your scalp, between your toes, your back, your buttocks. Take photos of new or changing spots. Compare them month to month.
Apps like UV Index by QSun can alert you when UV levels are high. But they don’t replace looking at your skin. One Reddit user found a 0.4mm melanoma because the app reminded him to check a spot he’d ignored for months. That’s the kind of moment that changes everything.
High-risk people - fair skin, 50+ moles, family history - should see a dermatologist every 3 to 6 months. But here’s the problem: the average wait for a dermatology appointment is nearly 30 days. In rural areas, it’s over two months. That’s why teledermatology is growing. In 2024, 61% of dermatology practices offered virtual visits. Accuracy is 87% - close to in-person. But Medicare pays less for virtual visits. That’s holding back access.
How Melanoma Is Treated
Treatment depends entirely on how far it’s spread.
- Stage 0 (in situ): Only in the top layer of skin. Surgery with a 0.5-1 cm margin around the mole is usually all you need. Cure rate: nearly 100%.
- Stage I-II: Deeper in the skin. Wider excision (1-2 cm) plus a sentinel lymph node biopsy (SLNB) if the tumor is over 0.8 mm. SLNB checks if cancer has reached nearby lymph nodes. If it hasn’t, you’re likely cured with surgery alone. Five-year survival: 97% for Stage IA.
- Stage III: Cancer reached lymph nodes. Surgery plus adjuvant therapy - drugs like nivolumab, pembrolizumab, or ipilimumab - to kill any leftover cells. These are immunotherapies that help your immune system find and destroy cancer. Side effects can be serious, but they’re manageable. Survival rates jump from 40% to over 70% with these drugs.
- Stage IV: Spread to distant organs. This is where things get complex. Two main paths: immunotherapy or targeted therapy.
Immunotherapy (like nivolumab + ipilimumab) works for more people. In the CheckMate 067 trial, 52% of patients were still alive five years later. Side effects? About 14% had severe reactions.
Targeted therapy (like dabrafenib + trametinib) only works if you have a BRAF mutation - about half of all melanomas do. It works faster - tumors shrink in weeks. But side effects are worse: 57% get serious issues like fever, rash, or liver problems. And resistance often develops after a year or two.
Both cost $150,000-$200,000 a year. Insurance helps, but out-of-pocket costs still hit $28,500 for some. That’s why so many patients on Reddit talk about financial toxicity. Treatment can bankrupt you even with coverage.
In early 2025, the FDA approved two new tools: an AI-powered dermoscopy tool called DermEngine’s VisualizeAI (93.2% accurate) and a personalized mRNA vaccine (mRNA-4157/V940) that cuts recurrence risk by 44% when combined with pembrolizumab. These aren’t cures yet - but they’re turning melanoma into a chronic, manageable disease for more people.
Why Some People Are Left Behind
Not everyone has equal access. In Mississippi, there’s only 1 dermatologist for every 100,000 people. In Massachusetts, it’s 7.8. That gap means people in rural or low-income areas are 22% more likely to be diagnosed with late-stage melanoma.
Black patients make up just 2% of melanoma cases - but 12% of those diagnosed at Stage III or IV. Why? Because lesions on darker skin are often mistaken for bruises, scars, or fungal infections. One patient, DJohnson_MD, had a spot on his foot called a “bruise” for over a year. It was Stage III acral melanoma.
And while the CDC spent $1.8 billion treating melanoma in 2024, they spent $0.02 per person on prevention. That’s not a mistake. It’s a failure.
What You Can Do Today
You don’t need to be a doctor to save your life. Here’s your action plan:
- Apply broad-spectrum SPF 30+ every morning. Reapply every 2 hours if you’re outside.
- Do a full-body skin check once a month. Use mirrors. Take photos.
- Know your ABCDEs. If something looks new, changing, or weird - get it checked.
- If you’re high-risk (fair skin, many moles, family history), see a dermatologist every 3-6 months.
- Never use a tanning bed. Not even once.
- Teach your kids. Make sun safety part of your daily routine - like brushing your teeth.
Survival isn’t about being lucky. It’s about being informed. Melanoma is beating us - but only if we let it. The tools to stop it are already here. We just need to use them.
Can melanoma be cured if caught early?
Yes. When melanoma is caught before it spreads beyond the top layer of skin (Stage 0 or IA), the five-year survival rate is over 99%. Surgery alone is often enough to cure it. That’s why monthly self-checks and annual dermatologist visits matter.
Do I need to check moles I’ve had for years?
Yes. Melanoma doesn’t always appear as a new mole. Many start as existing moles that change. Look for the E in ABCDE - evolving. If a mole gets darker, larger, starts itching, bleeding, or crusting - get it checked, even if it’s been there for 10 years.
Is sunscreen enough to prevent melanoma?
Sunscreen helps, but it’s not enough on its own. You also need shade, protective clothing, and avoiding peak sun hours. A single application of SPF 30 doesn’t block all UV rays, and people often miss spots like ears, necks, and feet. Combine sunscreen with other habits for real protection.
Can people with dark skin get melanoma?
Yes. While less common, melanoma in people with darker skin often appears in areas not exposed to the sun - under nails, on palms, soles of feet, or inside the mouth. It’s also more likely to be diagnosed late because it’s overlooked. Everyone needs to check their entire body, not just sun-exposed areas.
Are new treatments making melanoma less deadly?
Yes. Five years ago, Stage IV melanoma had a 20% five-year survival rate. Today, with immunotherapy and new vaccines, it’s over 50%. These treatments aren’t perfect - they’re expensive and can have side effects - but they’re turning melanoma from a death sentence into a manageable condition for many.
How often should I see a dermatologist?
If you’re average risk - no family history, fewer than 25 moles, no sunburns - one full-body exam every year is enough. If you’re high risk - fair skin, many moles, history of sunburns, or family history - go every 3 to 6 months. Don’t wait for symptoms. Early detection is your best defense.

ellen adamina
January 14, 2026 AT 14:47I used to ignore my moles until one started itching. Took a photo, compared it a month later-changed color. Went to the doc. Stage IA. Surgery done. No chemo. Just a scar and a new habit. Check your skin. Seriously.
Arjun Seth
January 16, 2026 AT 06:16People just don't care! Sunscreen? Please! If you're not burning, you're not getting any benefit! And tanning beds? That's just laziness! Why do you think they're still allowed? Because the government is in bed with big tanning! You think that's a coincidence?!
Nishant Garg
January 17, 2026 AT 23:47In India, we don't have the luxury of SPF 30+ in every pharmacy. But we do have neem oil, turmeric paste, and shade under banyan trees. My grandmother never used sunscreen. She lived to 92. Skin cancer? Rare. Maybe the answer isn't just chemicals-it's culture, rhythm, and respect for the sun, not fear of it.
Also, melanoma under nails? My uncle had it. We thought it was dirt. Took two years to diagnose. He lost a toe. We didn't know. No dermatologist for 100 miles. So yes-education matters. But so does access.
Nicholas Urmaza
January 19, 2026 AT 16:01If you're not checking your skin monthly you're not serious about living. Period. Sunscreen alone is a joke. You need hats. You need UV shirts. You need to treat your skin like your car-protect it every single day. No excuses. Your life is worth more than your tan.
RUTH DE OLIVEIRA ALVES
January 20, 2026 AT 01:45It is imperative to recognize that disparities in dermatological access are not merely logistical but deeply systemic. The disparity in dermatologist-to-population ratios between Massachusetts and Mississippi reflects broader inequities in healthcare infrastructure. Furthermore, the underfunding of prevention initiatives-$0.02 per person-constitutes a profound public health failure that demands immediate policy intervention.
Jan Hess
January 21, 2026 AT 18:10My dad had melanoma. Stage III. Took him 6 months to get in to see a specialist. He was lucky. I started doing monthly checks after that. Took pics of every mole. Now I show them to my kids. We do it together every Sunday after shower. It's our thing. Simple. But it saves lives.
Diane Hendriks
January 22, 2026 AT 13:44Why is this even a problem? Because we let foreigners and liberal bureaucrats dictate our health. The real cause? Too much fake sunscreen with chemicals that cause cancer. Real sun is good. Real skin is strong. If you're getting melanoma, maybe you're just weak. Stop blaming the sun. Take responsibility.
Tom Doan
January 22, 2026 AT 16:52So let me get this straight-you’re telling me that a $200,000/year drug that gives you a 52% five-year survival rate is better than… what? A $0.50 bottle of sunscreen? And yet we spend billions on chemo and nothing on prevention? That’s not science. That’s capitalism. And it’s disgusting.
Sohan Jindal
January 24, 2026 AT 10:49They’re hiding the truth. The sun doesn’t cause melanoma. It’s the 5G towers. And the fluoride. And the CDC’s secret agenda to make everyone dependent on drugs. You think they’d spend billions on treatment if they didn’t profit from it? Wake up. Your skin is fine. Stop being scared. They want you afraid.
Mike Berrange
January 24, 2026 AT 14:35Yeah, but have you ever tried to get a dermatology appointment in rural Ohio? I waited 87 days. My spot was already 3mm by then. And the AI tool? It flagged it as benign. Turns out it was Stage II. So now I’m not just mad at the system-I’m mad at the tech that’s supposed to help.
Dan Mack
January 26, 2026 AT 01:42So the government says to check your skin, but won’t pay for the doctors. They say sunscreen works, but don’t regulate the crap in it. They say AI helps, but then deny insurance for it. And now they want a vaccine? Please. This isn’t medicine. This is a pyramid scheme with melanoma at the top.