When a mole starts to change - growing unevenly, turning black, or itching without reason - it’s not just a skin issue. It could be melanoma, the deadliest form of skin cancer. But here’s the thing: if caught early, your chances of surviving are nearly 100%. If it spreads? That number drops to just over 32%. The gap between life and death isn’t just about time. It’s about detection. And treatment. And the quiet revolution happening right now in dermatology clinics, labs, and even people’s homes.
Why Melanoma Is Different
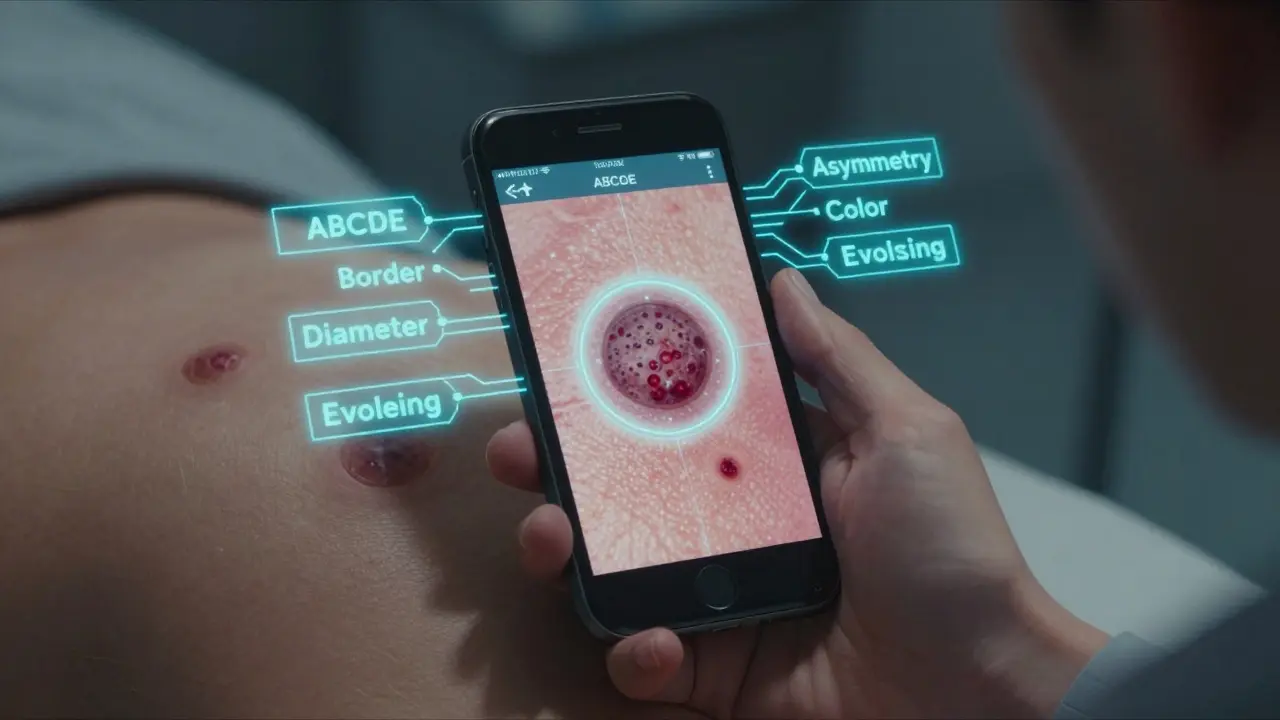
Melanoma doesn’t behave like other skin cancers. It grows fast. It spreads even faster. It starts in melanocytes - the cells that give your skin color - and can sneak into lymph nodes or organs before you even notice anything wrong. That’s why it accounts for less than 2% of all skin cancers but causes nearly 80% of skin cancer deaths. The good news? Most melanomas are visible. They show up on your skin. That means you, your doctor, or even a smart device can spot them before they become dangerous. The challenge? Not everyone knows what to look for. And not every doctor has the tools to tell a harmless mole from a deadly one.What to Look For: The ABCDE Rule (Still Works)
You don’t need a fancy machine to start saving your life. Just know the ABCDEs:- A - Asymmetry: One half doesn’t match the other.
- B - Border: Jagged, blurred, or irregular edges.
- C - Color: Multiple shades of brown, black, red, white, or blue.
- D - Diameter: Larger than 6mm (about the size of a pencil eraser).
- E - Evolving: Changing in size, shape, color, or texture over weeks or months.
How Doctors Are Seeing What the Eye Can’t
A visual exam is the first step. But it’s not enough. That’s where dermoscopy comes in - a handheld magnifier with polarized light that lets doctors see below the skin’s surface. It’s like switching from a flashlight to a microscope. But even dermoscopy has limits. Studies show primary care doctors catch only 60-70% of melanomas. Dermatologists do better - around 85% - but they’re not everywhere. That’s where AI is stepping in. In 2025, AI tools are now FDA-approved and being used in clinics across the U.S., Europe, and Australia. One system, called SegFusion, developed at Northeastern University, combines two neural networks: one to outline the mole, another to classify it. It hits 99% accuracy in research settings. Another, the iToBoS full-body scanner, takes six minutes to scan your entire skin, flagging 100+ spots with risk levels. It even explains why it flagged each one - something doctors need to trust it. Then there’s DermaSensor. It’s a pen-like device that shines near-infrared light on a mole and measures how the light scatters. It’s been cleared by the FDA for use by nurses and family doctors. In trials, it improved detection confidence by 87%. But here’s the catch: its specificity is low - only 26-40%. That means it flags a lot of harmless moles as suspicious. More biopsies. More stress. More cost.The Real Problem: Bias in the Machine
AI doesn’t see skin the way humans do. It sees pixels. And if the data it learned from mostly came from light-skinned people, it won’t recognize melanoma on darker skin as well. A 2025 JAMA Dermatology study found AI tools perform 12-15% worse on skin types V and VI. That’s not a small gap. That’s life or death. A melanoma on a Black patient is often diagnosed 2-3 years later than on a white patient. That delay cuts survival rates in half. Researchers are trying to fix this. The SegFusion team oversampled dark-skin images. The iToBoS project includes diverse datasets from 18 countries. But it’s not enough. Until every training dataset reflects the full range of human skin, AI will keep failing the people who need it most.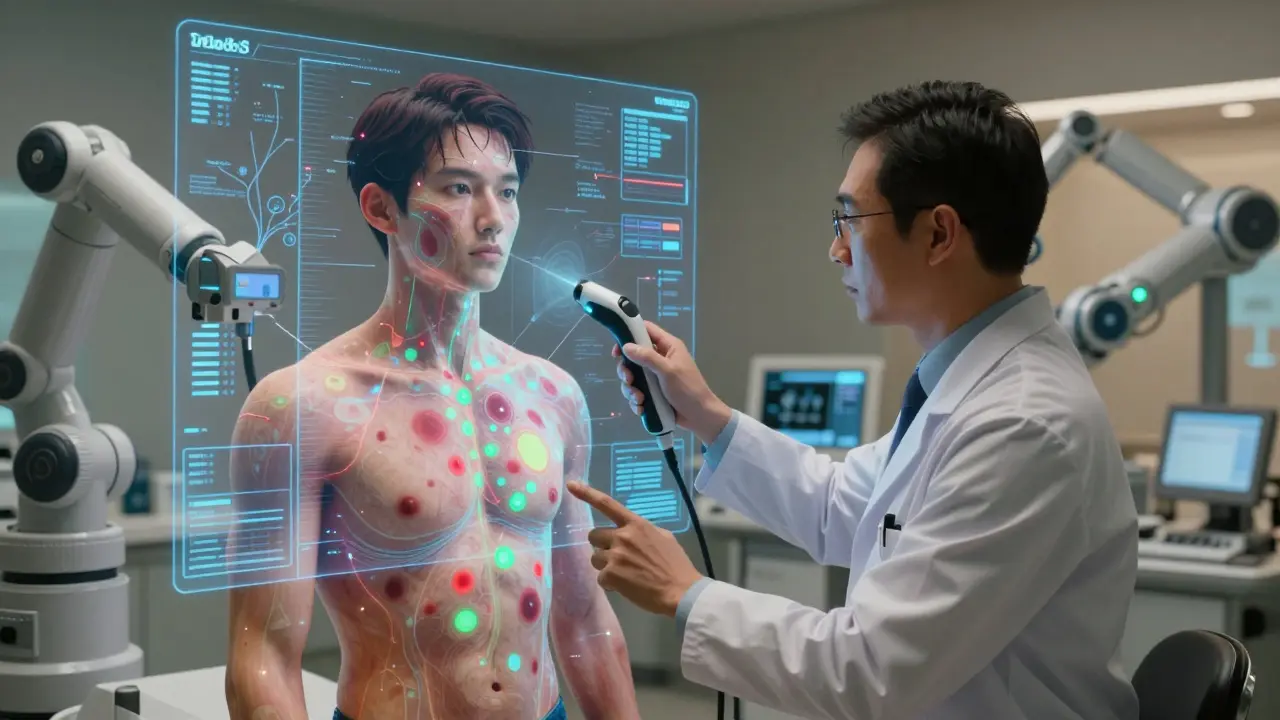
What’s Coming Next: Wearables and At-Home Screening
Imagine a patch you wear for a few days. It doesn’t need a battery. It doesn’t need Wi-Fi. It just sits on your skin and measures electrical differences between normal tissue and cancer. That’s what researchers at Wake Forest developed. In a small test with 10 people, it detected clear differences in lesions that turned out to be melanoma. The next version will use conductive hydrogel to stick better. The goal? A device you can use at home - like a glucose monitor for skin cancer. It’s not ready yet. But it’s coming. And when it is, it could change everything. People in rural areas. People without easy access to dermatologists. People who don’t know what to look for. They’ll get a signal - not a diagnosis - but a warning. And that’s enough to get them to a doctor.When Melanoma Spreads: The Immunotherapy Revolution
If melanoma spreads - to lymph nodes, lungs, liver, or brain - it used to mean a death sentence. Five years ago, survival was under 10%. Today? It’s over 50%. The reason? Immunotherapy. These drugs don’t kill cancer directly. They wake up your immune system. For years, your body knew the melanoma was there - but it didn’t act. Immunotherapy removes the brakes. The first big win was ipilimumab (Yervoy), approved in 2011. It targeted CTLA-4, a protein that stops immune cells from attacking. Then came pembrolizumab (Keytruda) and nivolumab (Opdivo), which block PD-1. Now, doctors use them together - or with newer drugs like fianlimab (targeting LAG-3) - and the results are stunning. In a 2025 trial, a new cell therapy called IMA203 PRAME helped 56% of patients with advanced melanoma achieve complete remission. That means no detectable cancer left. Some patients have stayed in remission for over five years. These aren’t miracles. They’re science. And they’re working.The Catch: Side Effects and Cost
Immunotherapy isn’t magic. It can cause your immune system to attack your own organs - leading to colitis, hepatitis, thyroid issues, or even heart inflammation. These side effects are manageable - but they require close monitoring. And the cost? One cycle of Keytruda can run $15,000. A full year? Over $100,000. Insurance covers it for approved cases, but not everyone qualifies. And not every country can afford it. In Australia, the PBS (Pharmaceutical Benefits Scheme) covers these drugs for eligible patients. In the U.S., it’s a patchwork. In low-income countries? Still out of reach.
What Works Best Right Now?
Here’s what the data says for 2026:| Method | Accuracy | Specificity | Who Uses It | Best For |
|---|---|---|---|---|
| Visual Exam (Primary Care) | 60-70% | 65-75% | General doctors | Initial screening |
| Dermoscopy | 80-85% | 80-90% | Dermatologists | High-risk moles |
| SegFusion AI | 99% | 87% | Dermatology clinics | Confirming suspicious lesions |
| DermaSensor (ESS) | 85-95% | 26-40% | Nurses, GPs | Low-resource settings |
| Combination Immunotherapy | N/A | N/A | Advanced melanoma patients | Metastatic disease |
There’s no single best tool. The best approach is layered: check your skin. See your doctor. Use dermoscopy if available. Let AI help confirm. And if it’s advanced? Get on immunotherapy fast.
What Patients Are Saying
On Reddit’s r/dermatology, people are split. One user wrote: “I used the iToBoS scanner at my clinic. It found a spot my dermatologist missed. I had it removed. It was Stage 1. I’m alive because of it.” Another said: “I got flagged for three moles that turned out to be nothing. I spent $1,200 on biopsies and two weeks of anxiety. I’m not doing it again.” The truth? Technology is powerful - but it’s not perfect. It’s a tool. Not a replacement for judgment. Not a replacement for care.The Future: Personalized Risk, Not Just Detection
The next frontier isn’t just finding melanoma. It’s predicting who will get it. Researchers are now combining:- AI skin scans
- Genetic markers (like CDKN2A mutations)
- UV exposure history
- Blood biomarkers
- Immune system profiles
What You Can Do Today
You don’t need a scanner. You don’t need a PhD. You just need to act.- Check your skin every month. Use a mirror. Take photos.
- Know your ABCDEs. If something changes - get it checked.
- Don’t skip your annual skin exam - even if you think you’re fine.
- Ask your doctor: “Do you use dermoscopy? Do you use AI tools?”
- If you have a family history of melanoma, get genetic counseling.
- Wear sunscreen. Not just at the beach. Every day.
The tools are here. The science is proven. Now it’s up to you - and your doctor - to use them.
Can melanoma be cured if caught early?
Yes. When melanoma is caught before it spreads beyond the top layer of skin (Stage 0 or Stage I), the 5-year survival rate is over 99%. Surgery to remove the mole is often all that’s needed. No chemo. No immunotherapy. Just early action.
Is AI better than a dermatologist at detecting melanoma?
In controlled studies, AI systems like SegFusion and DenseNet-201 match or slightly exceed dermatologist accuracy - especially on standard dermoscopy images. But real-world use is different. Dermatologists use context: your history, family risk, lesion location, and how it changed over time. AI doesn’t. The best results come when AI supports the doctor - not replaces them.
Why do some AI tools have low specificity?
Low specificity means the system flags too many harmless moles as cancerous. This happens because AI models are trained on datasets that don’t fully represent real-world skin variations - especially in lighting, angles, and skin tones. Some tools, like DermaSensor, prioritize sensitivity (catching all cancers) over specificity (avoiding false alarms). That’s good for safety - but bad for patient stress and healthcare costs.
Are immunotherapy treatments available everywhere?
No. In countries with universal healthcare like Australia, Canada, and the UK, key immunotherapies are covered by public programs. In the U.S., coverage depends on insurance and diagnosis stage. In many low-income countries, these drugs are unaffordable. Access remains a major barrier to survival - even when the science works.
Can I rely on smartphone apps to check for melanoma?
No. Apps that claim to diagnose melanoma from phone photos are not FDA-approved and lack clinical validation. Lighting, camera quality, and angle make results unreliable. Some apps have misclassified melanomas as benign. Always see a doctor - don’t trust an algorithm on your phone.
How often should I get a skin check?
If you have no risk factors, once a year is enough. If you’ve had melanoma before, have many moles, a family history, or fair skin - get checked every 6 months. High-risk patients should also do monthly self-checks. Don’t wait for symptoms. Melanoma doesn’t always itch or bleed.