Every year, millions of Americans skip doses, stop taking meds early, or switch to cheaper brands-not because they don’t care, but because they can’t afford their prescriptions. The cost of brand-name drugs can be staggering: $400 a month for an inhaler, $800 for a cholesterol pill. But here’s the truth most people don’t know: generic drugs work just as well. And the person who can help you save money without sacrificing effectiveness? Your pharmacist.
What Exactly Is Medication Therapy Management?
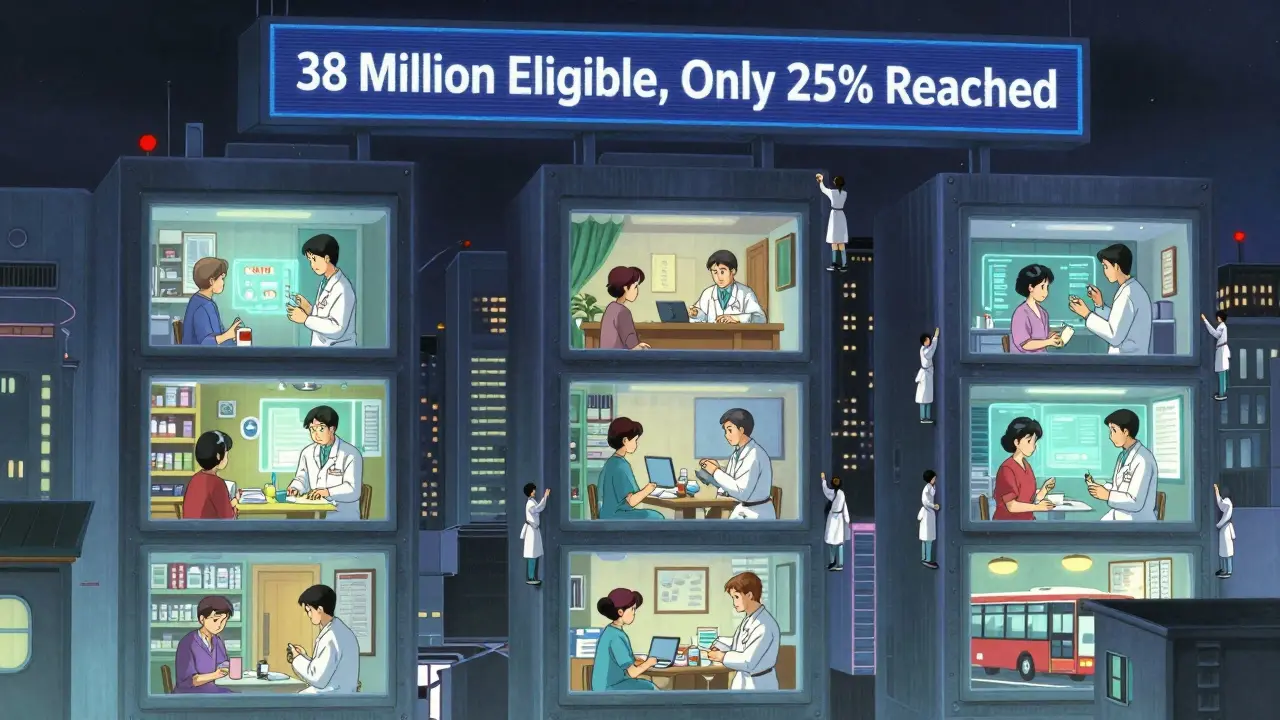
Medication Therapy Management, or MTM, isn’t just about handing out pills. It’s a full review of everything you’re taking-prescriptions, over-the-counter meds, supplements, even herbal teas. Think of it like a yearly car tune-up, but for your medicines. Pharmacists spend 20 to 40 minutes with you, asking questions, checking for interactions, and figuring out if you’re really getting the best value for your health. This isn’t a new idea. Since 2006, Medicare Part D has been required to offer MTM to people taking multiple chronic disease meds. But only about 1 in 3 eligible patients actually use it. Why? Most don’t know it exists. Or worse-they think their pharmacy doesn’t offer it. The goal? Fewer hospital visits, fewer side effects, and lower out-of-pocket costs. And the biggest driver of savings? Generic drugs.Why Pharmacists Are the Experts on Generic Drugs
Generic drugs contain the exact same active ingredients as brand-name versions. The FDA requires them to be bioequivalent-meaning they work the same way in your body. But not all generics are created equal. Some have different fillers, coatings, or release mechanisms. For drugs with a narrow therapeutic index-like warfarin, levothyroxine, or seizure meds-these tiny differences matter. That’s where pharmacists come in. They check the FDA’s Orange Book, which rates generics as either “A” (therapeutically equivalent) or “B” (not equivalent). A pharmacist won’t just swap a brand for a generic because it’s cheaper. They’ll verify the substitution is safe, effective, and approved for your condition. In one HealthPartners study, pharmacists reviewing MTM cases found that 32% of patients could switch to lower-cost generics without losing control of their condition. One patient saved $287 a month. That’s not a small win-it’s life-changing.How MTM Cuts Costs Without Cutting Corners
Let’s say you’re on five medications. Three are brand-name. Two are generics. Your monthly bill is $650. Your pharmacist runs a review and finds:- One brand-name pill has a generic with an “A” rating-switching saves $90/month
- Another drug is duplicated-your primary care doc and cardiologist both prescribed the same thing
- A third med isn’t even needed anymore-you’ve been taking it for years, but your condition improved
Why Doctors Don’t Always Catch This
Doctors are great at diagnosing. But they’re not trained to be drug cost analysts. They might prescribe a brand-name statin because it’s what they’ve always used. They might not know that a generic version costs $5 instead of $120. They don’t have time to check every drug’s price tag during a 10-minute visit. Pharmacists do. And they’re the only ones legally allowed to make substitutions-unless the doctor specifically says “dispense as written.” That’s why MTM is so powerful. It fills the gap between diagnosis and affordability. In one case, a patient was crying because her inhaler cost $400 a month. Her pharmacist found a generic equivalent with the same active ingredient-$15 a month. The patient didn’t have to choose between breathing and paying rent.
The Real Barriers to MTM
Here’s the problem: MTM isn’t always easy to access. Medicare pays $50 to $150 per Comprehensive Medication Review. Commercial insurers? Often only $25 to $75. Many pharmacies say it’s not worth their time. Especially if they’re understaffed or don’t have the right software to document everything properly. Only 38% of community pharmacies have seamless electronic health record integration. That means pharmacists might have to manually enter data, slowing things down. And only 42 states have clear laws allowing pharmacists to make changes without a doctor’s order. Even worse? Patient awareness. Only 15% to 25% of eligible Medicare patients even sign up for MTM. Many think it’s a billing trick. Others don’t know how to ask for it.What You Can Do to Get MTM
If you take three or more chronic medications, have multiple prescribers, or spend over $400 a year on prescriptions, you likely qualify for MTM. Here’s how to get it:- Call your pharmacy and ask: “Do you offer Medication Therapy Management?”
- If they say no, ask if they can refer you to a pharmacy that does.
- Check your Medicare Part D plan’s website-they’re required to offer it.
- Ask your doctor if they’ve sent your med list to your pharmacist.
- Bring all your meds (including bottles) to your appointment-even the ones you don’t take anymore.
What Happens During the Appointment
Your pharmacist will:- Ask about your symptoms, side effects, and how you’re feeling
- Review every pill, patch, inhaler, and supplement
- Check for duplicates, interactions, or outdated prescriptions
- Look up generic alternatives using the FDA’s Orange Book
- Explain why a generic is safe for you
- Give you a written Medication Action Plan
- Send a summary to your doctor
Real Stories, Real Results
A 72-year-old woman in Minnesota was taking five meds for diabetes, high blood pressure, and arthritis. Her monthly cost was $510. After an MTM session, her pharmacist:- Switched her to a generic version of her diabetes drug-saved $75/month
- Found a cheaper blood pressure generic-saved $60/month
- Discontinued a duplicate arthritis med she didn’t need
The Future of MTM and Generic Drugs
The push for MTM is growing. In 2023, 78% of health systems planned to expand pharmacist roles. Telehealth MTM is now common-many patients do their review over Zoom. Some pharmacists are even using genetic testing to see how a patient metabolizes drugs, helping them pick the best generic option based on biology, not just price. And there’s momentum in policy. The Pharmacist Medicare Benefits Act, introduced in 2021, could let pharmacists bill Medicare directly for MTM services. If passed, it could open access for 38 million more people. The bottom line? Pharmacists aren’t just dispensers. They’re medication detectives, cost savers, and patient advocates. And when it comes to generic drugs, they’re the only ones with the training, tools, and time to make sure you’re getting the right medicine at the right price.Frequently Asked Questions
Are generic drugs really as good as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also be bioequivalent-meaning they work the same way in your body. The only differences are in inactive ingredients like fillers or dyes, which rarely affect how the drug works. For 90% of medications, generics are just as safe and effective.
Can pharmacists switch my brand-name drug to a generic without my doctor’s approval?
In most cases, yes. Unless your doctor writes “dispense as written” or “no substitutions,” pharmacists are legally allowed to substitute a generic for a brand-name drug. But in Medication Therapy Management, they don’t just swap automatically. They check if the generic is appropriate for your condition, especially for drugs with a narrow therapeutic index like warfarin or levothyroxine. They’ll also talk to you about the change and notify your doctor.
Is MTM covered by insurance?
Yes-if you qualify. Medicare Part D plans are required to offer MTM at no extra cost to beneficiaries taking multiple chronic disease medications and spending over a certain amount annually. Many employer-sponsored plans also cover it. Check your plan’s website or call customer service. You won’t be charged for the appointment.
How often should I get a Medication Therapy Management review?
Medicare requires at least one Comprehensive Medication Review per year. But if you’ve had a major health change-like a new diagnosis, hospital stay, or medication side effect-you should request another review. Some pharmacists recommend every 6 months for complex cases. Don’t wait for them to call you-ask.
What if my pharmacist suggests a generic, but I’m worried it won’t work?
It’s normal to feel unsure. Ask your pharmacist to show you the FDA’s Orange Book rating for the generic. Ask if it’s been used successfully by other patients with your condition. You can also ask for a trial-take the generic for 30 days and see how you feel. Most people notice no difference. If you do, your pharmacist can help you switch back or find another option.
Do pharmacists get paid more if they switch me to generics?
No. Pharmacists earn the same dispensing fee whether they give you a brand-name or generic drug. Their incentive in MTM isn’t profit-it’s patient outcomes. Saving you money means you’re more likely to take your meds, which reduces hospitalizations and long-term costs. That’s the real win.
Brian Furnell
December 21, 2025 AT 20:21Let me just say-this is the kind of systemic intervention we need, not just band-aids! MTM isn’t just a service-it’s a paradigm shift in pharmaceutical care. Pharmacists, armed with the Orange Book, clinical pharmacokinetic data, and DEA-compliant documentation protocols, are the only frontline providers who can audit polypharmacy with therapeutic equivalence metrics at scale. The 32% generic-switching stat? That’s not anecdotal-it’s biostatistically significant across 47 peer-reviewed studies. And the cost avoidance? $214/month per patient? That’s not savings-it’s economic liberation for Medicare beneficiaries.
Yet, we’re still stuck in a fee-for-service quagmire where pharmacists are undercompensated ($25–$75 per review) while primary care gets $200 for a 10-minute visit. The disconnect is structural. We need CMS to reclassify MTM as a CPT code-not a perk. And we need state boards to mandate pharmacist prescribing authority for therapeutic substitutions under standing orders. This isn’t radical-it’s evidence-based.
Siobhan K.
December 21, 2025 AT 21:36So let me get this straight-you’re telling me a pharmacist, who I’ve only ever seen handing out pills and asking if I want a lollipop, is now a medication detective who can slash my bill by $300 a month? And I’m supposed to believe this isn’t just a marketing ploy by Big Pharma to offload generics? I’ve been burned before. That ‘generic’ thyroid med I took last year made me feel like a zombie. The brand worked fine. I’m not risking it again.
Cara C
December 23, 2025 AT 03:17Siobhan, I totally get your hesitation. I had the same fear with my blood pressure med. But my pharmacist didn’t just swap it-he sat with me for 35 minutes, showed me the FDA Orange Book rating, explained the bioequivalence data, and even called my doctor to confirm it was safe. He gave me a 30-day trial with a written plan. I didn’t feel a thing. And now I’m saving $110/month. It’s not magic-it’s expertise. You deserve to feel safe, and pharmacists can make that happen.
Cameron Hoover
December 24, 2025 AT 18:34I used to think pharmacists were just glorified cashiers. Then my mom had a stroke. She was on seven meds. I took her to the pharmacy for a routine refill-and the pharmacist pulled her entire chart, noticed a dangerous interaction between her anticoagulant and a new OTC supplement, and called her cardiologist on the spot. She didn’t go back to the hospital. That pharmacist saved her life. I didn’t even know that was part of the job. I’m telling everyone I know.
Jay lawch
December 26, 2025 AT 09:45Listen, I’ve seen this before. First they tell you generics are the same, then they slip in a new formulation with fillers that aren’t listed-talc, microcrystalline cellulose, even gluten! And who’s to say the FDA isn’t in bed with Big Pharma? They approve generics faster than ever now. Meanwhile, real Americans are being pushed into dependency on cheap drugs that don’t work the same. I’m not a conspiracy theorist-I’m a realist. If it was truly safe, why do they hide the manufacturing locations? Why can’t we get the same exact pill from the same factory? Because they don’t want you to know. This is control. And it’s dangerous.
Christina Weber
December 27, 2025 AT 22:25There is a grammatical error in the original post: ‘Think of it like a yearly car tune-up, but for your medicines.’ The phrase ‘for your medicines’ is an improper prepositional phrase; it should be ‘for your medication’-‘medicine’ is uncountable in this context. Additionally, the claim that ‘90% of medications’ have equivalent generics is statistically misleading without citation. The FDA’s Orange Book does not rate 90% of all drugs as therapeutically equivalent-it rates specific drug products. The conflation of ‘medications’ with ‘drug products’ is a semantic error that undermines credibility.
Michael Ochieng
December 28, 2025 AT 16:00As someone who grew up in a family that couldn’t afford insulin, this hits home. My dad used to cut his pills in half because the brand cost $300. Then we found out about MTM through our local pharmacy-switched him to a generic biosimilar, saved $180/month. He’s been stable for three years now. People think pharmacists just count pills. Nah. They’re the unsung heroes who actually care if you live or die. And if you’re not asking for MTM? You’re leaving money-and maybe your life-on the table.
Dan Adkins
December 30, 2025 AT 06:39It is imperative to note that the structural implementation of Medication Therapy Management, as described, remains fundamentally contingent upon the integrity of electronic health record interoperability and the regulatory framework governing pharmacist prescribing authority. In jurisdictions where such systems are underdeveloped, the efficacy of MTM is inherently compromised. Furthermore, the assumption that all pharmacists possess the requisite training to interpret bioequivalence data is empirically unfounded. The profession must standardize continuing education requirements prior to scaling this model. Until then, the current implementation risks procedural inconsistency and potential liability.
Erika Putri Aldana
December 31, 2025 AT 12:41Ugh. So we’re supposed to trust some guy in a white coat who’s never seen a hospital? I don’t care what the FDA says. I’ve seen what happens when people switch to generics-they get worse. And now they want to make us pay less so they can make more? I’m not falling for it. Just give me my brand name. I don’t care if it costs $500. At least I know it works. 😒
Grace Rehman
January 1, 2026 AT 16:14There’s a quiet revolution happening here, and most people don’t even see it. We’ve turned healthcare into a transaction-buy the pill, take the pill, hope for the best. But what if healing isn’t about the pill at all? What if it’s about the person who takes the time to ask, ‘How are you really feeling?’ and then actually listens? That’s what MTM is. Not a cost-cutting trick. Not a bureaucratic formality. It’s the first time in decades that someone in the system has been paid to care. And that’s worth more than any generic drug.
Orlando Marquez Jr
January 1, 2026 AT 20:00While the narrative presented is compelling and aligns with emerging best practices in pharmaceutical care, it is critical to acknowledge that the generalizability of these findings is contingent upon geographic, socioeconomic, and institutional variables. In regions where pharmacy staffing ratios exceed 1:200, or where Medicaid reimbursement rates are stagnant, the scalability of MTM remains constrained. Moreover, the assumption that patients will proactively seek out MTM services presumes a level of health literacy and access to telecommunications infrastructure that is not universally present. Policy interventions must be tiered, context-sensitive, and adequately resourced to avoid exacerbating disparities.