When your blood sugar climbs above 180 mg/dL, your body starts sending warning signs-often too quietly to notice until it’s too late. Hyperglycemia isn’t just a number on a glucometer. It’s a silent crisis that can creep up over days or explode in hours, leading to coma, hospitalization, or worse. For people with diabetes, understanding the early signs and knowing exactly what to do when blood sugar hits 300, 400, or even 600 mg/dL isn’t optional-it’s life-saving.
What Exactly Is Hyperglycemia?
Hyperglycemia means your blood glucose is too high. It happens when insulin-your body’s key to unlocking cells for glucose-isn’t working right. In type 1 diabetes, your body doesn’t make insulin at all. In type 2, your cells stop listening to it. Either way, sugar piles up in your bloodstream instead of fueling your muscles and brain. The American Diabetes Association defines mild hyperglycemia as 180-250 mg/dL, moderate as 251-300 mg/dL, and severe as anything above 300 mg/dL. But numbers alone don’t tell the whole story. What matters is how your body reacts.
Early Warning Signs You Can’t Ignore
Most people wait until they feel awful before checking their blood sugar. That’s a mistake. The earliest symptoms are subtle, easy to brush off as stress, fatigue, or just getting older. But if you notice any of these consistently, test immediately:
- Urinating more than usual-especially at night. You might be going to the bathroom every hour, with large volumes. This is your body trying to flush out excess sugar.
- Extreme thirst that doesn’t go away, even after drinking a full glass of water. You might find yourself drinking 4 liters or more a day.
- Blurry vision. Sugar pulls fluid from your lenses, making focus hard. It’s not an eye problem-it’s a blood sugar problem.
- Unexplained fatigue. Even after a full night’s sleep, you feel drained. Your cells aren’t getting the fuel they need.
A 2023 survey by the ADA found that 68% of people with diabetes experienced blurred vision during hyperglycemic episodes. Yet, 67% of patients on DiabetesDaily.com didn’t act until their blood sugar was already over 300 mg/dL. Don’t wait for the worst.
When It Gets Worse: The Intermediate Stage
If your blood sugar stays above 250 mg/dL for more than a few hours, symptoms escalate. Headaches, trouble focusing, and unexplained weight loss start showing up. You might lose 5% or more of your body weight in a few weeks-not from dieting, but because your body is breaking down fat and muscle for energy. This happens because glucose can’t enter your cells, so your body thinks it’s starving.
A 2021 study in JAMA Internal Medicine found that 47% of type 2 diabetes patients had difficulty concentrating during moderate hyperglycemia. That’s not laziness-it’s your brain struggling without glucose. If you’re suddenly forgetting appointments, struggling to read a menu, or feeling foggy during conversations, check your sugar. It could be the cause.
The Emergency Phase: DKA and HHS
When blood sugar climbs above 300 mg/dL, you’re in danger. Two life-threatening conditions can develop: diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS). They’re different, but both need emergency care.
DKA mostly affects people with type 1 diabetes. It kicks in fast-within 24 to 48 hours. Your body starts burning fat for energy, producing toxic ketones. Symptoms include:
- Deep, fast breathing (Kussmaul respirations)-your body trying to blow off acid
- Fruity-smelling breath-like nail polish remover or overripe fruit
- Nausea, vomiting, and stomach pain
- Confusion or drowsiness
DKA is a medical emergency. Left untreated, it can lead to coma or death. The mortality rate is 1-5%, but it’s higher in kids and people who delay care.
HHS is more common in type 2 diabetes and creeps up over days or weeks. Blood sugar often exceeds 600 mg/dL. You’re severely dehydrated-your body has lost 8 to 12 liters of fluid. Symptoms include:
- Extreme weakness or drowsiness
- Loss of consciousness
- High fever
- Weak or rapid pulse
HHS has a higher death rate-15-20%-especially in older adults. Why? Because it often goes unnoticed until the person is already in a coma. A 2021 NIH study found that patients over 65 with HHS had a 22% mortality rate.

What to Do When Blood Sugar Is Too High
If your blood sugar is above 240 mg/dL, don’t just take more insulin and hope for the best. Follow this step-by-step:
- Check for ketones. Use a urine test strip or a blood ketone meter. If ketones are moderate or high, do not exercise. You could make it worse.
- Drink water. 8-16 ounces every hour. Sugar-free fluids only. No soda, juice, or sweet tea.
- Take your correction dose. Use your insulin-to-carb ratio or your doctor’s recommended correction factor. Most people need 0.1 units per kilogram of body weight every hour until sugar drops.
- Recheck your blood sugar every 2-3 hours. If it doesn’t drop by 50-100 mg/dL after an hour of insulin, call your doctor. You may need IV fluids or hospital care.
- Don’t skip meals. Even if you feel sick, eat small amounts of carbs. Your body needs fuel to recover.
One big mistake? Insulin stacking. Taking another dose too soon because your sugar hasn’t dropped yet. That can crash your blood sugar into hypoglycemia. The FDA warns that 33% of insulin pump users have made this error. Wait at least 3 hours between doses unless your doctor says otherwise.
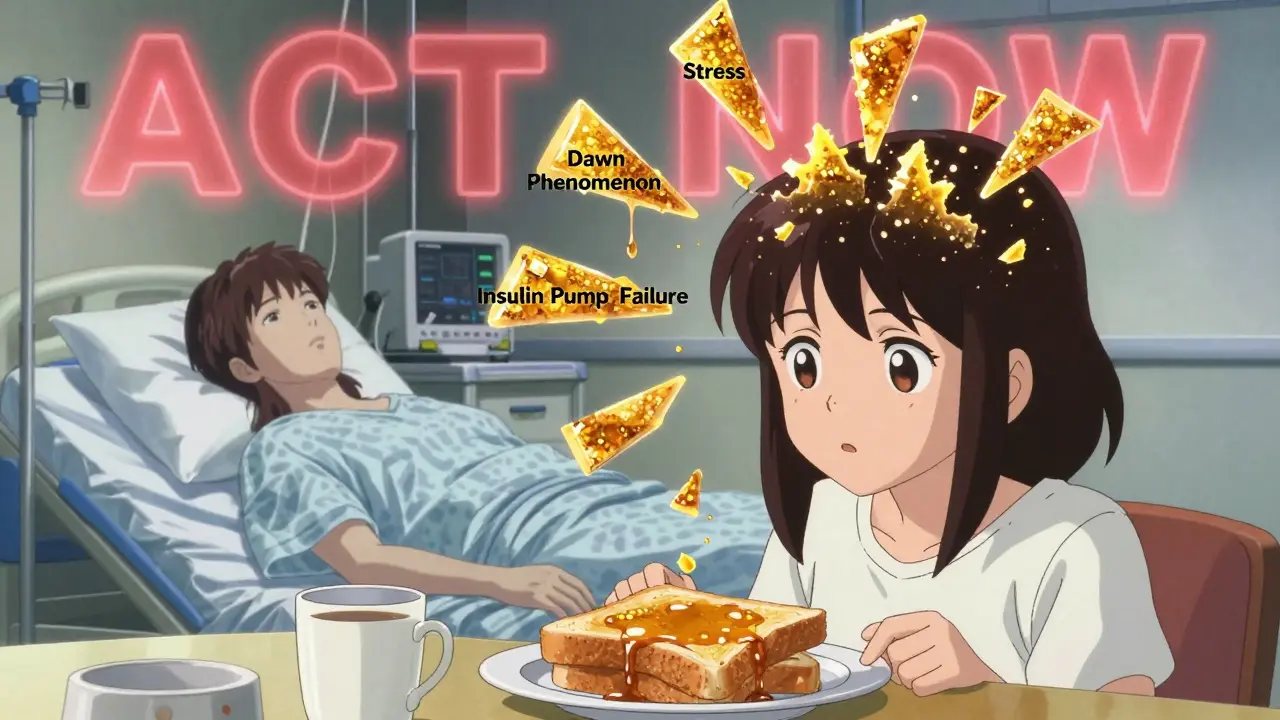
Common Triggers You Might Not Realize
Why does your blood sugar spike out of nowhere? Here are the top causes:
- Illness (42% of cases): Infection, fever, or even a cold can raise cortisol and adrenaline, which push sugar up.
- Insulin pump failure (18%): A clogged catheter or disconnected tubing can stop insulin delivery. Always check your pump before you panic.
- Carb-counting errors (29%): A single slice of pizza or a hidden sugar in sauce can throw off your balance.
- Emotional stress (11%): Anxiety, grief, or even a fight with a loved one can trigger a hormonal surge.
- The dawn phenomenon: Between 4 and 8 a.m., your body releases hormones that naturally raise blood sugar. If your morning levels are consistently high, your basal insulin may need adjusting.
One patient in Melbourne shared on Reddit that her blood sugar spiked every Sunday morning. She thought it was her weekend breakfast. Turns out, it was the dawn phenomenon. Her endocrinologist adjusted her basal rate by 25%, and her numbers stabilized.
How Technology Is Changing the Game
Continuous glucose monitors (CGMs) are no longer luxury devices-they’re lifesavers. A 2023 Dexcom study showed CGM users reduced severe hyperglycemia episodes by 57%. Why? Real-time alerts. You get a vibration on your phone when your sugar hits 250 mg/dL, before you even feel symptoms.
In January 2024, the FDA approved Dexcom G7’s new “Glucose Guardian” algorithm. It predicts a spike 30 minutes before it happens. That’s huge. You can drink water, take insulin, or pause a meal before your sugar goes off the charts.
But tech only works if you use it. A 2023 JAMA Internal Medicine study found that 19% of people with repeated hyperglycemia had undiagnosed gastroparesis-delayed stomach emptying that messes with insulin timing. If your sugar spikes hours after eating, ask your doctor about this.
When to Call 911 or Go to the ER
Don’t wait. If you or someone you care for has:
- Blood sugar above 600 mg/dL
- Confusion, drowsiness, or can’t wake up
- Vomiting and can’t keep fluids down
- Strong fruity breath with rapid breathing
- Loss of consciousness
Call emergency services immediately. HHS and DKA don’t wait for appointments. Time is tissue. Every hour counts.
Prevention Is Possible
Studies show that structured education reduces emergency visits by 42%. That means learning your triggers, testing regularly, and knowing your insulin doses. The CDC’s Diabetes Self-Management Education program has helped thousands. If you’re unsure where to start, call the American Diabetes Association’s 24/7 hotline. They handled over 12,000 calls last month.
And if you’re worried about cost: Medicare now covers CGMs for most people with diabetes. The $1,200 annual price tag is no longer a barrier for many. Talk to your doctor. There are programs, discounts, and even manufacturer assistance.
Final Thought: It’s Not About Perfection
Hyperglycemia isn’t a failure. It’s a signal. Even the most experienced people with diabetes have spikes. What matters is how you respond. Test early. Act fast. Know your numbers. And never ignore the quiet signs-because by the time you feel awful, it’s already too late.
What blood sugar level is considered dangerous?
A blood sugar level above 240 mg/dL is a warning sign that you need to act. Above 300 mg/dL is considered severe and requires immediate insulin and hydration. Above 600 mg/dL is a medical emergency, often signaling hyperosmolar hyperglycemic state (HHS), which can lead to coma or death if untreated.
Can you have high blood sugar without having diabetes?
Yes. Severe stress, infections, steroid medications (like prednisone), or conditions like Cushing’s syndrome can cause temporary hyperglycemia in people without diabetes. Pancreatitis or pancreatic cancer can also damage insulin-producing cells. If someone without diabetes has repeated high readings, they need testing for underlying conditions.
How do I know if it’s DKA or HHS?
DKA usually happens in type 1 diabetes and comes on fast. You’ll have ketones in your blood or urine, fruity breath, nausea, and deep breathing. HHS is more common in type 2 diabetes, develops slowly over days, and features extreme dehydration, confusion, and very high blood sugar (often over 600 mg/dL) with little to no ketones. Blood tests are needed to confirm, but if you’re confused or unconscious, treat it as an emergency regardless.
Should I exercise if my blood sugar is high?
Only if your blood sugar is below 250 mg/dL and you have no ketones. If your sugar is above 250 mg/dL and ketones are present, exercise can make your blood sugar rise even higher by releasing more stored glucose. Wait until your levels come down and ketones are gone before getting active.
Why does my blood sugar spike in the morning?
This is called the dawn phenomenon. Between 4 a.m. and 8 a.m., your body naturally releases hormones like cortisol and growth hormone, which raise blood sugar to prepare for the day. This affects everyone, but people with diabetes can’t compensate with enough insulin. Adjusting your nighttime basal insulin or eating a lower-carb dinner can help. A 2022 study found that adjusting basal insulin by 20-30% reduced morning spikes in 74% of patients.
Can stress cause high blood sugar?
Yes. Stress triggers your body’s fight-or-flight response, releasing adrenaline and cortisol. These hormones tell your liver to dump glucose into your bloodstream. Even emotional stress-like an argument, grief, or work pressure-can raise your sugar by 50-100 mg/dL. Managing stress through sleep, breathing exercises, or counseling can help stabilize your levels.
What should I do if I can’t reach my doctor during a high blood sugar emergency?
If your blood sugar is over 300 mg/dL and you have symptoms like vomiting, confusion, or trouble breathing, go to the nearest emergency room immediately. Don’t wait for a call back. Hospitals are equipped to treat DKA and HHS with IV fluids and insulin. Delaying care increases the risk of coma or death. If you’re unsure, call 911.
