Walking up to the pharmacy counter with your prescription in hand feels like the last step in getting better. But what if the medicine you’re about to take could make you sicker? That’s why confirming allergies and drug interactions at pickup isn’t just a formality-it’s a lifesaving check. Every year, nearly 7% of hospital admissions are caused by preventable adverse drug events, many of which happen because someone didn’t catch an allergy or interaction before the pill was handed over.
Why This Check Matters More Than You Think
You might think your doctor already checked for allergies when they wrote the prescription. Maybe they did. But here’s the problem: patient records are often outdated. A 2023 study from the University of Michigan found that over one-third of allergy entries in electronic health records are older than five years. Someone might have been told they’re allergic to penicillin as a kid, but never got tested again. Turns out, 90% of those people aren’t truly allergic. Still, the system flags it-and now you can’t get the best antibiotic for your infection. Or maybe you’re on three medications, and your doctor added a fourth without realizing one of them boosts the risk of a dangerous drop in blood pressure. These interactions don’t always show up on paper. That’s why the pharmacist has to do the final verification-right before you walk out the door.The Four-Step Verification Process Pharmacists Use
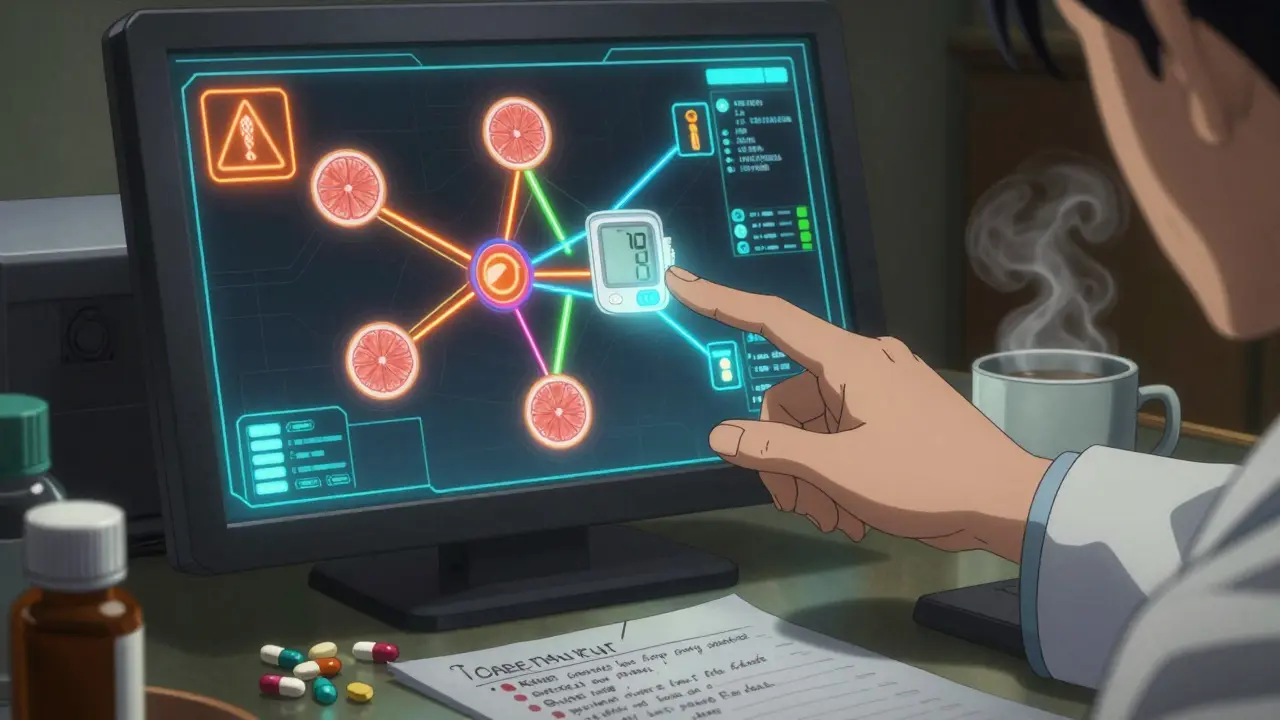
By law, pharmacists must complete a safety check before dispensing any medication. In Australia, this is guided by the Therapeutic Goods Administration (TGA) and aligns with global standards from the American Society of Health-System Pharmacists (ASHP). The process takes less than 90 seconds, but it’s packed with critical steps:- Confirm current allergy documentation - The system pulls up your recorded allergies. If it’s been more than 12 months since your last update, the pharmacist will ask: "Has anything changed? Did you get a rash after taking amoxicillin last year?"
- Run a drug interaction check - The pharmacy system cross-references your meds with Lexicomp or Micromedex databases. These tools flag over 1,000 known drug-drug interactions, 300+ drug-food interactions, and 2,000+ drug-condition conflicts. For example, taking statins with grapefruit juice can cause muscle damage. The system doesn’t just say "interaction"-it tells you how serious it is.
- Check for inactive ingredient triggers - Some people aren’t allergic to the active drug, but to the dye, filler, or preservative in it. If you’re allergic to sulfites, you need to know if your tablet contains sodium metabisulfite. If you’re sensitive to lactose, your pill might be made with it. Pharmacists now use picklists that filter out false alarms from common ingredients like aspartame or titanium dioxide.
- Document and confirm - The pharmacist types a note: "Allergy confirmed with patient. No interactions detected. Patient advised to avoid grapefruit with simvastatin." That note goes into your record and is visible to every provider who accesses it.
What You Can Do to Help
You’re not just a passive recipient here. You’re part of the safety team. Here’s how to make this step work better for you:- Keep a written list - Write down every medication you take, including supplements and OTC drugs. Include the reason you take them. Bring this list to every appointment and pharmacy visit.
- Be specific about allergies - Don’t just say "I’m allergic to penicillin." Say: "I broke out in hives and had trouble breathing after taking amoxicillin in 2019." That helps the pharmacist know if it’s a true allergy or just a rash.
- Ask questions - If the pharmacist says, "There’s an interaction with your blood pressure med," ask: "What does that mean for me? Should I watch for dizziness?"
- Update your records - If you’ve had a new reaction, had an allergy test, or stopped a medication, tell your pharmacist. Don’t assume they’ll know.
Common Pitfalls and How to Avoid Them
Even with the best systems, mistakes happen. Here are the top three problems-and how to spot them:- False alarms - You get an alert because your medicine contains a dye. But you’ve taken it before with no issue. Don’t just accept the warning. Ask: "Is this really a risk for me?" Many systems now let pharmacists suppress alerts for known non-reactions.
- Outdated records - Your file says you’re allergic to sulfa drugs, but you’ve taken Bactrim without a problem for years. Tell the pharmacist. They can override the flag with a note-and you’ll be safer next time.
- Missing interactions - Your new antidepressant might interact with a supplement you bought online. Pharmacists can’t see everything. If you’re taking something from a health store, tell them. Even "natural" doesn’t mean safe.
Technology Is Helping-But It’s Not Perfect
Most pharmacies use systems connected to electronic health records, like Epic or Cerner. These tools can flag over 99% of real interactions. But they also generate too many false alerts. A 2024 study found pharmacists ignore nearly 7 out of 10 allergy warnings-because so many are meaningless. Newer systems are getting smarter. Epic’s 2024 update now prioritizes alerts based on severity. If you have five allergies, it won’t bother you with low-risk ones. Google Health’s pilot program used AI to scan doctor’s notes and found 32% more undocumented allergies. That’s huge. But tech alone won’t fix this. The Mayo Clinic found that when pharmacists took just two extra minutes to talk to patients at pickup, inappropriate antibiotic substitutions dropped by 37%. That’s not because of software. It’s because someone asked, "How did you react the last time you took this?"
What Happens If Something Goes Wrong?
If you take a medicine and feel unwell-rash, swelling, trouble breathing, chest pain-stop taking it and call your doctor or go to the ER. But also, call the pharmacy. Tell them what happened, what you took, and when. They’ll update your record and flag it for future prescriptions. Pharmacists are required to report serious adverse events to national safety agencies. In Australia, that’s the TGA. Your report helps improve safety for everyone.What’s Changing in 2026?
By the end of 2025, the FDA will require all drug labels to use standardized formats that clearly list allergens and interaction risks. That means your pill bottle might say: "Contains sulfites. May interact with blood pressure meds. Avoid grapefruit." In 2026, Medicare and private insurers in Australia will start penalizing pharmacies with high override rates for allergy alerts. That means pharmacists will be under more pressure to get it right-and they’ll be more likely to stop and talk to you. The future is AI-driven. Systems will soon analyze your past prescriptions, lab results, and even your pharmacy visit history to predict risks before you even walk in. But for now, the best tool is still a pharmacist who listens.What should I do if I think my allergy is wrong?
Tell your pharmacist and ask if you can be referred for an allergy test. Many people who think they’re allergic to penicillin aren’t. Skin testing can confirm this-and open up better treatment options. Don’t assume your label is correct. It might be keeping you from the best medicine.
Can I trust the pharmacy’s system to catch every interaction?
Most systems catch over 99% of serious interactions, but they miss things you take outside the system-like herbal supplements, vitamins, or alcohol. Always tell your pharmacist about everything you’re using. Even if it’s "natural," it can interact.
Why do I keep getting alerts for ingredients I’ve taken before?
Some systems flag all inactive ingredients-even ones that rarely cause reactions. If you’ve taken a medication with lactose or FD&C red dye before without issues, tell your pharmacist. They can update your profile to suppress those alerts in the future.
What if the pharmacist doesn’t ask me about allergies?
Don’t wait for them to ask. Say: "I want to make sure this is safe with my allergies." Pharmacists are trained to verify, but they rely on you to provide accurate info. If you’re uncomfortable, go to another pharmacy. Your safety isn’t optional.
How often should I update my allergy list?
Update it every time you see a new doctor or pharmacist, or after any new reaction. Even if you feel fine, write it down. A rash, stomach upset, or dizziness after taking a drug could be an early sign. Keep a note on your phone or in your wallet.

Damario Brown
January 15, 2026 AT 02:44so i took amoxicillin last year and got a rash but i didnt think it was a big deal now im scared to take any antibiotic lmao
John Pope
January 15, 2026 AT 13:30the system is a goddamn circus. they flag everything-lactose, titanium dioxide, even the fucking ink on the pill-and then act like they did their job. meanwhile, real risks slip through because we’re drowning in noise. it’s not safety-it’s performative compliance. the pharmacist’s time is being wasted on alerts that mean nothing while the real dangers go unchecked. we need AI that learns from actual patient outcomes, not just database entries written in 2012.
Avneet Singh
January 16, 2026 AT 22:07the entire pharmacovigilance infrastructure is a relic of analog-era thinking. you're relying on static, siloed EHRs in a world where polypharmacy is the norm. the TGA guidelines are noble but syntactically obsolete. what we need is a dynamic, federated ontology-something that can parse unstructured clinical notes and correlate longitudinal exposure data. until then, we're just rearranging deck chairs on the Titanic.
Adam Vella
January 17, 2026 AT 08:52It is imperative to note that the current protocol, while commendable in intent, lacks sufficient standardization across jurisdictions. The variance in documentation practices between Epic and Cerner systems, for instance, introduces critical inconsistencies. Furthermore, the reliance on patient self-reporting without corroboration via serological testing constitutes a systemic vulnerability. A mandatory, algorithmically triggered referral pathway for suspected false-positive allergies should be implemented nationwide.
Nelly Oruko
January 18, 2026 AT 16:05i’ve been keeping a handwritten list since my last hospital stay. it’s in my purse, on my phone, even printed and taped to my fridge. i tell every pharmacist: "i’m allergic to sulfa, but not penicillin, and i take turmeric for my knees." they always look surprised. like it’s too much to ask. it’s not. it’s basic.
Vinaypriy Wane
January 20, 2026 AT 11:57Wait-you mean the pharmacist isn’t supposed to just assume? You mean they’re supposed to actually talk to you? Like, real human conversation? I didn’t know that was part of the job. I thought they just scanned the barcode and handed you the bottle like a vending machine. This whole thing feels… weirdly personal. And honestly? Kinda beautiful.
Diana Campos Ortiz
January 21, 2026 AT 12:48my grandma used to say "if it don't feel right, it ain't right"-and she never took a pill without asking the pharmacist what it was for. i do that now. even if i know. because sometimes, they catch something i forgot. like when i was on that new blood pressure med and didn't realize grapefruit was in my juice. they stopped me. i owe them my life.
Adam Rivera
January 23, 2026 AT 05:07in my country, we don’t even get this level of check. my cousin got prescribed a drug that interacted with his diabetes med-he almost went into a coma. the pharmacy just shrugged and said, "doctor ordered it." we need this system everywhere. not just in the US. not just in Australia. everywhere.
Trevor Davis
January 24, 2026 AT 15:51so like… i’m allergic to penicillin? or not? i’ve taken it like 5 times. no problem. but my chart says "anaphylaxis" from 2011. i asked my doc to remove it. they said "we can’t just delete it." why? because bureaucracy? because someone once typed it wrong? i’m not a database entry. i’m a person. fix the damn system.
John Tran
January 26, 2026 AT 00:50let me tell you something about this whole thing-it’s not about the drugs, it’s about control. the pharmaceutical industry wants you to believe that the system is foolproof so you don’t question the pills they’re pushing. the real danger isn’t the interaction-it’s the fact that we’ve outsourced our health to algorithms written by people who’ve never held a sick person’s hand. the pharmacist asking you if you had a rash? that’s the last human moment before the machine takes over. and we’re letting it happen. we’re letting them turn medicine into a checklist. and when the machine fails-and it will-no one’s gonna be there to hold you while you gasp for air.
Trevor Whipple
January 27, 2026 AT 00:55you people are so naive. you think the pharmacist gives a crap? they’re paid by the hour. they scan, they click, they move on. if you don’t ask, you’re dead. i’ve seen it. i told a pharmacist my kid was allergic to sulfa-he said "cool" and handed me the bottle. i had to yell. you think tech fixes this? no. YOU have to be the fucking enforcer. stop waiting for someone else to save you.
Lethabo Phalafala
January 28, 2026 AT 15:17my sister died because no one asked. she had a rash after amoxicillin at 8. they never tested her. 25 years later, they gave her a drug with the same chemical structure. she went into anaphylaxis in the ER. they didn’t even check her file properly. I’m not just angry-I’m furious. If you’re taking meds, talk. If you’re giving them, ask. Don’t wait for the system to save you. Save each other.
Lance Nickie
January 29, 2026 AT 04:10the whole "4-step process" is a lie. i’ve been to 3 pharmacies. none of them did step 3. none. they just asked if i was allergic to penicillin. that’s it. the rest is marketing.
sam abas
January 31, 2026 AT 02:59you’re all missing the point. the real issue isn’t the allergies or the interactions-it’s that pharmacists are overworked, underpaid, and forced to run 100 checks per hour. the system isn’t broken. it’s being murdered by capitalism. when your paycheck depends on speed, not safety, you’re gonna ignore 7 out of 10 alerts. it’s not negligence. it’s survival. fix the pay. fix the hours. then maybe the tech will matter.
Angel Tiestos lopez
February 1, 2026 AT 14:59❤️ this is why i love my local pharmacist. she remembers my name, my dog’s name, and that i hate blue dyes. she’s not just a pharmacist-she’s my health guardian. if we could clone her, we’d cure the whole system. 🙏