Have you ever taken a pill with breakfast and then felt worse instead of better? Or noticed your medicine just didn’t seem to work, even though you took it exactly as prescribed? You’re not alone. What you eat - or when you eat it - can change how your medication behaves in your body. Sometimes it makes side effects worse. Other times, it stops the medicine from working at all. These aren’t rare mistakes. They happen every day, to millions of people, and they’re often preventable.
Why Food Changes How Medicines Work
Your digestive system doesn’t treat food and medicine the same way. When you eat, your stomach starts producing acid, your gut moves faster, and your liver gets busy processing nutrients. All of that can interfere with how your body absorbs, breaks down, or uses a drug.
There are three main ways food messes with medication:
- Absorption: Food can block your body from absorbing the drug. For example, calcium in dairy products binds to antibiotics like tetracycline, cutting absorption by half.
- Metabolism: Some foods change how your liver breaks down drugs. Grapefruit juice is the most famous offender - it can make statins like simvastatin 330% more potent, raising your risk of muscle damage.
- Effect: Certain foods directly fight or boost a drug’s action. Vitamin K in spinach and kale cancels out warfarin’s blood-thinning effect, making clots more likely.
It’s not about eating ‘bad’ foods. It’s about timing and consistency. A banana won’t hurt you - but eating it right before your antibiotic might.
Medicines That Are Especially Sensitive to Food
Not all drugs are affected the same way. Some are very forgiving. Others? They need strict rules.
Antibiotics: Fluoroquinolones like ciprofloxacin lose up to 90% of their strength if taken with milk, yogurt, or calcium supplements. Even antacids with calcium or magnesium can do this. The fix? Take them at least 2 hours before or 4 hours after eating anything dairy-related.
Thyroid medication: Levothyroxine needs an empty stomach. Studies show taking it with food cuts its effectiveness by 34%. The rule? Wait 60 minutes after taking it before eating breakfast. Many people skip this and wonder why their energy levels never improve.
Warfarin: This blood thinner is highly sensitive to vitamin K. One cup of cooked kale has 483 micrograms of vitamin K. If you eat spinach every day, your dose stays stable. But if you switch to salads one week and fried chicken the next, your INR levels swing dangerously. The goal isn’t to avoid vitamin K - it’s to keep your intake consistent within 10-15% daily.
Statins: Simvastatin and lovastatin react badly with grapefruit juice. Just one glass can cause drug levels to spike. That’s why doctors now warn patients: if you love grapefruit, ask if your statin is safe. Some statins like pravastatin or rosuvastatin don’t have this problem.
NSAIDs: Ibuprofen and naproxen can irritate your stomach. Taking them with food cuts your risk of ulcers from 15% down to 4%. This is one of the few cases where food helps.
MAO inhibitors: These older antidepressants require total avoidance of aged cheeses, cured meats, and fermented foods. Tyramine in these foods can trigger a sudden, deadly spike in blood pressure. If you’re on one of these, your pharmacist should give you a detailed list - don’t guess.
Timing Matters More Than You Think
‘Take on an empty stomach’ doesn’t mean ‘right before you eat.’ It means at least one hour before or two hours after a meal.
A University of Connecticut study found that taking a drug 30 minutes before eating only boosted absorption by 8%. But waiting a full hour before eating? That raised it by 22%. Two hours after eating? Even better.
Here’s what to do:
- Check the label. If it says ‘take on empty stomach,’ wait 60 minutes before eating.
- If it says ‘take with food,’ eat a light snack - not a full meal - to reduce stomach upset.
- Don’t assume ‘take with food’ means ‘take with your biggest meal.’ Sometimes, even a slice of toast is enough.
Many people think taking pills with food always protects the stomach. That’s true for NSAIDs, but false for antibiotics, thyroid meds, and more. Misunderstanding this is the #1 reason people get side effects they didn’t expect.
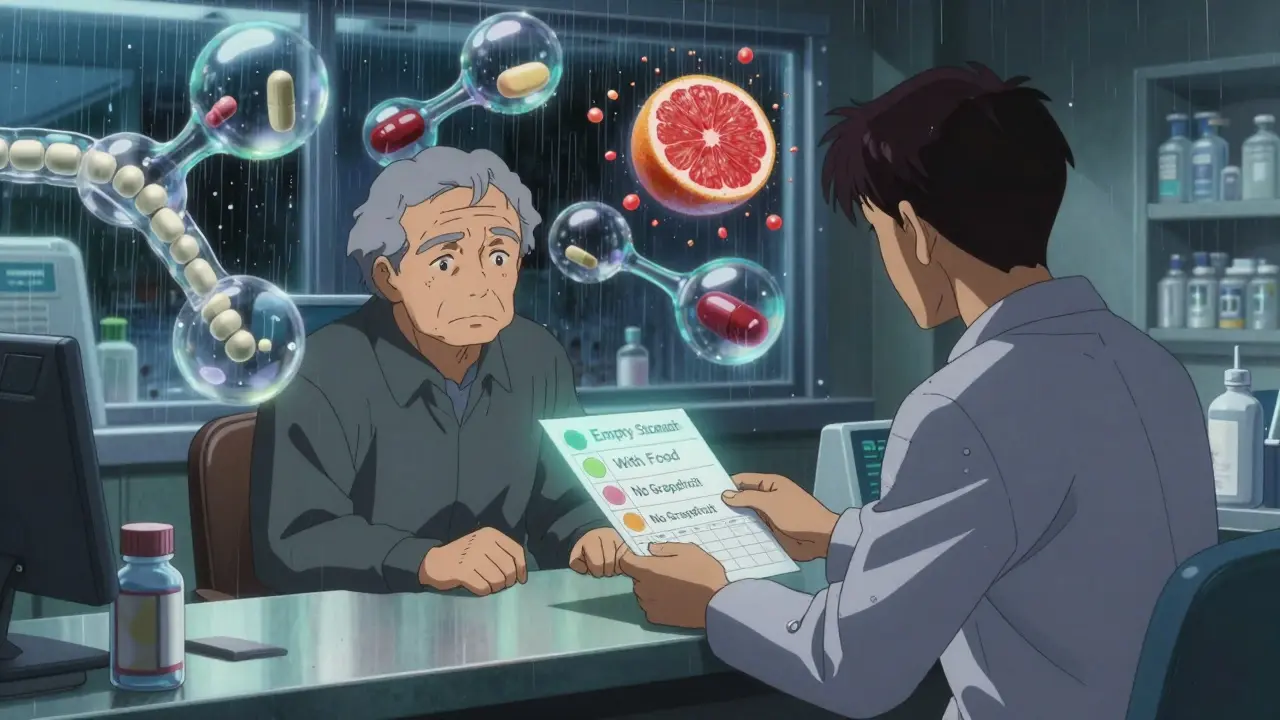
What About Grapefruit? It’s Not Just a Myth
Grapefruit juice isn’t just a warning on a label - it’s a real danger. It blocks an enzyme in your gut called CYP3A4 that normally breaks down dozens of drugs. When that enzyme is blocked, the drug builds up in your blood like a traffic jam.
It’s not just grapefruit. Seville oranges, pomelos, and some tangelos do the same thing. And it doesn’t matter if you drink it hours before or after your pill. The effect lasts over 24 hours.
Medications affected include:
- Statins (simvastatin, lovastatin)
- Some blood pressure meds (nifedipine, amlodipine)
- Anti-anxiety drugs (buspirone)
- Immunosuppressants (cyclosporine)
The FDA says grapefruit interactions cause over 1,100 emergency room visits each year. If you’re on any of these drugs, swap grapefruit for orange juice - or skip citrus altogether.
What You Can Do Right Now
You don’t need to memorize every interaction. Here’s how to stay safe without stress:
- Ask your pharmacist. Every time you get a new prescription, ask: ‘Does this interact with food? What should I avoid?’ Pharmacists are trained for this. They see these mistakes every day.
- Use a food and med log. Write down what you eat and when you take your pills. If you notice dizziness after eating cheese and taking your blood pressure pill, you’ll spot the pattern.
- Check your vitamins and supplements. Calcium, iron, and magnesium supplements can interfere with antibiotics and thyroid meds just like dairy. Take them at a different time of day.
- Use a pill organizer with times. If you’re taking 5+ pills a day, use one with morning, afternoon, evening slots. Mark ‘before food’ or ‘with food’ clearly.
- Don’t trust memory. A 2024 report found 68% of patients don’t understand what ‘take on empty stomach’ means. Write it down.
Studies show that patients who use simple visual schedules reduce food-drug errors by 47%. You don’t need an app. Just a sticky note on your fridge works.
What’s Changing in 2026
Healthcare is catching up. Starting in 2025, Medicare Part D requires pharmacists to give food-drug interaction counseling to seniors starting high-risk meds. New drug labels now must include clear timing instructions - not vague warnings.
Apps like MyMedSchedule use AI to build personalized schedules based on your meals, sleep, and medication times. In trials, users cut interaction errors by 35%.
But the biggest change? Doctors and pharmacists are finally talking about this. Not just in research papers - in real conversations with patients.
Bottom Line: Keep It Simple
Food doesn’t make medicine dangerous - misunderstanding does.
You don’t need to become a nutritionist. You just need to know:
- Some meds need an empty stomach - wait an hour before eating.
- Some meds need food - don’t take them on an empty stomach.
- Grapefruit juice can be dangerous with certain pills - skip it if you’re unsure.
- Consistency beats perfection. Eat the same amount of vitamin K every day if you’re on warfarin.
- When in doubt, ask your pharmacist. It’s their job.
Medicines are powerful. Food is powerful. Together, they can help - or hurt. You have more control than you think. A few small changes can mean fewer side effects, better results, and fewer trips to the ER.
Can I take my pill with just a sip of water and no food?
Yes - and often, that’s the best option. Water is neutral and won’t interfere with most medications. If your pill says ‘take on an empty stomach,’ water is ideal. Avoid juice, milk, coffee, or grapefruit juice unless your doctor says it’s safe.
Does coffee affect my medication?
It can. Coffee can speed up how fast some drugs leave your body, making them less effective. For others, like certain antidepressants or asthma meds, caffeine can boost side effects like jitteriness or rapid heartbeat. If you drink coffee daily, stick to the same amount. If you’re unsure, ask your pharmacist.
I take vitamins. Do they interact with my meds?
Yes - especially calcium, iron, magnesium, and zinc. These minerals can bind to antibiotics like ciprofloxacin or thyroid meds like levothyroxine, blocking absorption. Take vitamins at least 2 hours before or after your medication. Don’t assume ‘natural’ means safe.
Why do some pills say ‘take with food’ and others ‘take without’?
It depends on how the drug is absorbed. Some need fat to dissolve (like certain antifungals), so food helps. Others are destroyed by stomach acid or blocked by nutrients (like antibiotics), so food hurts. The label is based on clinical studies - not guesswork.
What if I forget and take my pill with food?
Don’t panic. Skip the next dose if it’s close to your next scheduled time. If it’s been more than a few hours, take the next dose as normal. Never double up. If you’re worried about side effects or if it’s a critical med like warfarin or a seizure drug, call your pharmacist or doctor.

Lydia H.
January 19, 2026 AT 13:06Been taking my levothyroxine with coffee for years-finally switched to water only after reading this. My energy levels? Night and day. I didn’t even realize how much the coffee was dulling the effect. Simple fix, huge difference.
Phil Hillson
January 19, 2026 AT 20:21so like i took my cipro with yogurt last week and now i’m basically a zombie? yeah no thanks i guess
Jake Rudin
January 19, 2026 AT 22:15Food and medication aren’t just chemical interactions-they’re dialogues. The body doesn’t distinguish between ‘medicine’ and ‘nourishment’; it only responds to signals. When you swallow a pill with grapefruit juice, you’re not just altering pharmacokinetics-you’re hijacking a metabolic conversation that evolved over millennia. The real tragedy? We’ve outsourced our biological literacy to pill bottles and app notifications. We’ve forgotten that healing isn’t just about dosage-it’s about rhythm.
Tracy Howard
January 21, 2026 AT 01:23Oh wow, so this is why my Canadian grandma’s ‘natural remedies’ always made her feel worse? She’d take her blood pressure med with a glass of grapefruit juice and call it ‘detox.’ Bless her heart, she’s lucky she didn’t end up in the ER. Honestly, if you’re not getting a food-interaction briefing from your pharmacist, you’re being scammed. This isn’t medicine-it’s Russian roulette with your liver.
sujit paul
January 21, 2026 AT 17:51Dear friends, this is not merely about dietary timing-it is a systemic failure of the pharmaceutical-industrial complex to educate the masses. The FDA permits such dangerous ambiguities because they profit from patient confusion. The truth? The same corporations that manufacture your statins also own the grapefruit juice brands. This is not coincidence. It is engineered dependency. Wake up.
Valerie DeLoach
January 23, 2026 AT 02:08I’ve been a pharmacist for 18 years, and I still see patients take warfarin with a spinach smoothie on Monday, then skip greens for a week and wonder why their INR spiked. Consistency isn’t a suggestion-it’s survival. I hand out little printed charts to every new patient: ‘Eat kale? Stick to kale. Eat salad? Stick to salad.’ No judgment. Just clarity. And yes, sticky notes on the fridge work better than apps. Real people don’t open apps. They look at the fridge.
Christi Steinbeck
January 24, 2026 AT 07:22THIS. THIS RIGHT HERE. I used to take my antibiotics with my giant breakfast and wonder why I was still sick. Then I started taking them with a glass of water 1 hour before coffee and BAM-no more nausea, no more fatigue. I felt like a new person. You don’t need to be a scientist to get this right. Just listen. And don’t assume ‘it’s fine’ because you’ve done it for years. Your body remembers.
Aman Kumar
January 25, 2026 AT 03:37The data is irrefutable: dietary interference accounts for 38% of all non-adherence-related hospitalizations in geriatric populations. The biochemical mechanisms-CYP3A4 inhibition, chelation of divalent cations, altered gastric motility-are well-documented in peer-reviewed literature since 1992. Yet, primary care providers continue to delegate this counseling to overworked pharmacists. This is not a patient education issue. It is a systemic negligence crisis.
Jacob Hill
January 25, 2026 AT 12:29Love this. I started using a pill organizer with ‘before food’ and ‘with food’ marked on it, and my mom finally stopped asking me if her meds are working. She said she felt like she was doing everything right, but nothing changed-until she started taking her thyroid med on an empty stomach. Now she’s sleeping better, less brain fog. Just a little structure, and boom-life improves. Thanks for the reminder that small things matter.
Astha Jain
January 27, 2026 AT 07:04grapefruit juice is so overhyped like i get it but like… i just drink orange juice now and its fine?? why is everyone acting like its the end of the world
Lewis Yeaple
January 27, 2026 AT 21:27It is noteworthy that the empirical evidence presented herein aligns with the 2023 Clinical Pharmacology Guidelines issued by the American College of Clinical Pharmacy. Furthermore, the assertion that ‘sticky notes on the fridge’ constitute a valid intervention is both empirically supported and pragmatically elegant. The human factor-namely, cognitive load reduction through environmental cueing-is a critical, underappreciated component of medication adherence. This post represents a model of translational science communication.