Hemochromatosis isn’t just about having too much iron-it’s about your body absorbing it when it shouldn’t. Left untreated, that extra iron doesn’t just sit around. It builds up in your liver, heart, pancreas, and joints, quietly causing damage you won’t feel until it’s too late. Most people don’t know they have it until they’re diagnosed with cirrhosis, diabetes, or heart problems. But here’s the truth: if caught early, hemochromatosis is one of the easiest genetic conditions to treat. And the treatment? Simple, cheap, and effective: blood removal. That’s right-phlebotomy, the same process used by blood donors, is the frontline defense against iron overload.
Why Your Body Can’t Handle Extra Iron
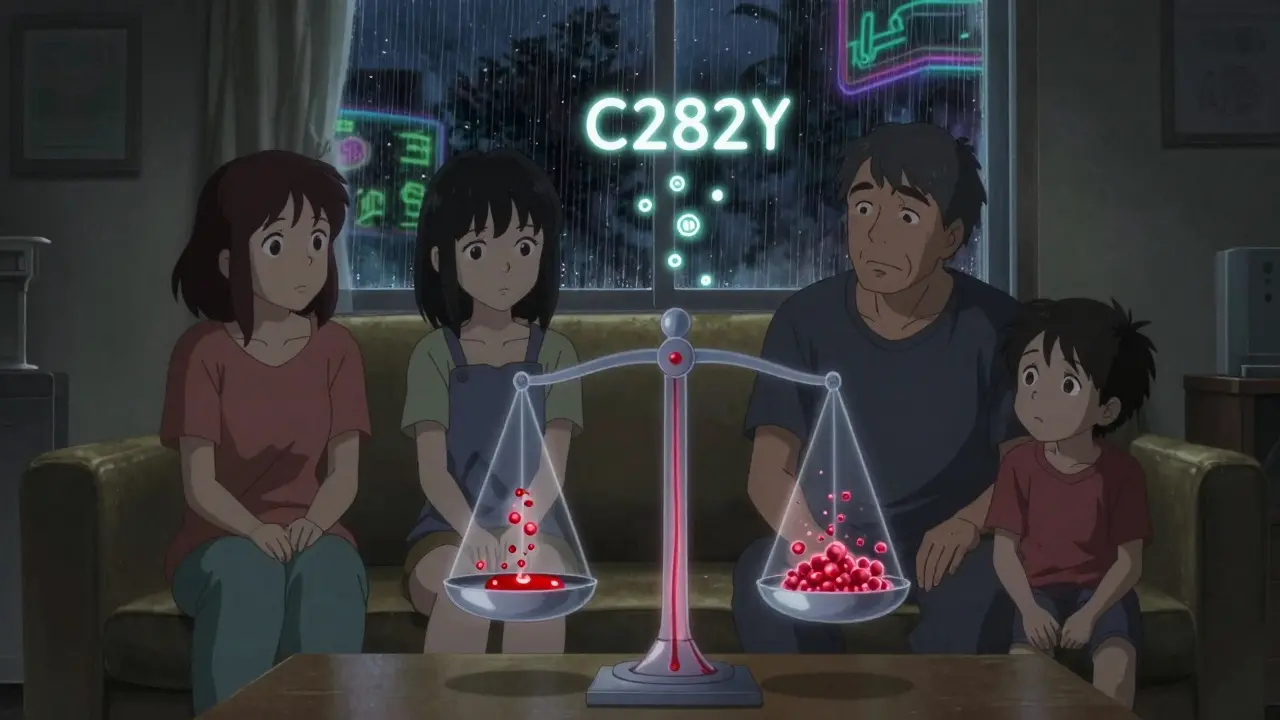
Everyone needs iron. It’s in your red blood cells, helping carry oxygen. But your body doesn’t have a natural way to get rid of excess iron. Normally, your liver makes a hormone called hepcidin that tells your gut to slow down iron absorption. In hemochromatosis, that signal breaks. A mutation in the HFE gene-most often the C282Y variant-stops hepcidin from working. So your gut keeps pulling in iron, even when you’ve had enough. Over time, you absorb 2 to 3 times more iron than you should. That’s 0.5 to 1 gram of extra iron every year. After 20 years? You could have 5 grams in your body. The average person only carries about 1 gram.
This isn’t about eating too much red meat. Even if you eat a low-iron diet, your body still overabsorbs. It’s a genetic flaw, not a lifestyle mistake. And it’s more common than you think. In people of Northern European descent-especially those with Irish, Scottish, or Welsh roots-about 1 in 83 carry two copies of the faulty gene. That’s the kind of risk that makes it the most common inherited disorder in those populations.
What Symptoms You Might Miss
Early hemochromatosis doesn’t scream for attention. It whispers. Fatigue? You blame it on stress. Joint pain? You think you’re getting older. Loss of libido? You chalk it up to aging or depression. These are the top three symptoms-and they show up in 65% to 74% of patients before any organ damage is visible.
By the time you notice your skin turning bronze or gray, your liver is already under siege. That’s not a tan-it’s iron staining your skin. Abdominal pain? That’s your liver swelling. Diabetes? That’s iron destroying your pancreas. And if you’re a man over 40 with unexplained heart rhythm problems, it could be iron building up in your heart muscle.
Women are protected for years because they lose iron through menstruation. But after menopause, their risk spikes. Many women are diagnosed only after their husbands or fathers are found to have it. That’s why family screening matters so much.
How Doctors Diagnose It
There’s no single test for hemochromatosis. It’s a two-step puzzle. First, blood tests. If your transferrin saturation is over 45% and your serum ferritin is above 300 ng/mL (or 200 ng/mL for women), that’s a red flag. Ferritin is the storage form of iron-when it’s high, your body is overloaded. Transferrin saturation tells you how much iron is floating in your blood. In secondary iron overload-like from too many blood transfusions-transferrin saturation is normal. In hemochromatosis? It’s sky-high. That’s the key difference.
Next comes genetic testing. If your blood tests look suspicious, you get tested for HFE mutations. The C282Y homozygous mutation (two bad copies) accounts for 80 to 95% of diagnosed cases. H63D or S65C mutations are less likely to cause serious problems on their own. A positive genetic test confirms the diagnosis. No liver biopsy is needed anymore. MRI scans can now measure liver iron accurately without surgery.
But here’s the problem: most doctors don’t think to order these tests. A 2023 study found only 12% of primary care doctors routinely check transferrin saturation in patients with fatigue or joint pain. That’s why the average patient sees five doctors over seven years before getting the right diagnosis. You can’t fix what you don’t diagnose.

Phlebotomy: The Treatment That Works
Phlebotomy is the gold standard. It’s simple: remove 450 to 500 milliliters of blood-about one unit-once a week. Each unit takes out 200 to 250 milligrams of iron. That’s more than your body absorbs in a week. The goal? Bring your ferritin down to between 50 and 100 ng/mL. For someone with ferritin at 2,000 ng/mL, that means 30 to 60 sessions. It can take a year or more.
It’s not glamorous. You’ll feel tired after each session. Your veins might be hard to find after a while. But it works. Studies show that if you start phlebotomy before your ferritin hits 1,000 ng/mL, you have a 99% chance of avoiding cirrhosis and liver cancer. Once you’re at target levels, you switch to maintenance: every 2 to 4 months, depending on how fast your iron builds back up. Most people need 4 to 6 treatments a year for life.
And it’s cheap. Each session costs $0 to $50 if done at a blood center that accepts therapeutic donations. Compare that to iron chelation drugs like deferasirox, which cost $25,000 to $35,000 a year. Chelation is only used when someone can’t tolerate phlebotomy-because of heart failure, severe anemia, or other reasons.
What Happens If You Don’t Treat It
Untreated hemochromatosis doesn’t just cause discomfort. It kills. Once ferritin climbs above 1,000 ng/mL, your risk of cirrhosis jumps to 50 to 75%. And once cirrhosis sets in, your 10-year survival rate drops to 60%. Liver cancer risk rises sharply. Heart failure, diabetes, and arthritis become common. Even if you don’t die from it, your quality of life plummets.
One patient from the Iron Disorders Institute described waiting eight years for a diagnosis. By then, his ferritin was 2,850 ng/mL. He needed 62 phlebotomies. He lost his job. He couldn’t play with his kids. He didn’t know he was sick until he was almost broken.
But here’s the flip side: another patient started treatment at ferritin 400 ng/mL. Within six months, his energy came back. His joint pain vanished. His liver enzymes normalized. He’s now on maintenance and feels better than he did in his 30s.
Living With Hemochromatosis
Once you’re on a maintenance schedule, life returns to normal. You can still eat red meat, drink alcohol in moderation, and live without restrictions. But there are a few things to avoid. Don’t take iron supplements. Don’t take vitamin C with meals-it boosts iron absorption. Don’t drink raw shellfish-it can carry bacteria that thrive in iron-rich blood and cause deadly infections.
Family screening is critical. If you’re diagnosed, your siblings and children should be tested. About 70% of cases are found through family screening after one person is diagnosed. Genetic testing now costs as little as $150. It’s worth it.
Many patients feel fine after a few months of phlebotomy and stop coming in. That’s a mistake. Iron builds back up slowly. Stopping treatment means you’re back on the path to organ damage. The goal isn’t to feel better-it’s to stay protected for life.
What’s Next for Treatment
Researchers are working on drugs that mimic hepcidin-the hormone your body can’t make. One experimental drug, PTG-300, has shown promise in early trials, reducing iron levels without needing blood removal. It’s not available yet, but it could change the game for people who can’t tolerate phlebotomy.
For now, though, the best tool we have is still the oldest: a needle and a bag. It’s not sexy. It’s not high-tech. But it’s free, safe, and proven to save lives. The real challenge isn’t finding a cure-it’s finding the people who need it before it’s too late.
Can hemochromatosis be cured?
No, hemochromatosis can’t be cured because it’s a genetic condition. But it can be completely managed. With regular phlebotomy, iron levels stay low, organs don’t get damaged, and life expectancy returns to normal. Treatment isn’t optional-it’s lifelong. Stop treatment, and iron builds back up.
Can you get hemochromatosis from eating too much iron?
No. Hemochromatosis is caused by a gene mutation, not diet. Even people who eat very little iron can develop severe iron overload if they have two faulty copies of the HFE gene. Diet doesn’t cause it, but it can make it worse. Avoiding iron supplements and vitamin C with meals helps slow down absorption.
Is phlebotomy safe?
Yes, phlebotomy is very safe when done properly. Each session removes about one unit of blood, similar to donating blood. Side effects are mild-dizziness, fatigue, or bruising at the site. Serious complications are rare. The bigger risk is not doing it. Untreated iron overload causes liver failure, heart disease, and diabetes.
Why do some people need more phlebotomies than others?
It depends on how much iron they’ve stored before treatment started. Someone with ferritin at 500 ng/mL might need 10 sessions. Someone at 3,000 ng/mL could need 60 or more. Age, gender, and how long the condition went undiagnosed also matter. Men tend to accumulate more iron earlier because they don’t lose blood through menstruation.
Should I get tested if my parent has hemochromatosis?
Yes. If one of your parents has the C282Y homozygous mutation, you have a 50% chance of being a carrier and a 25% chance of inheriting two faulty copies. Even if you feel fine, get your ferritin and transferrin saturation tested. Genetic testing is affordable and can prevent years of damage. Early detection is the only way to avoid serious complications.

Angel Tiestos lopez
January 13, 2026 AT 23:56bro i got diagnosed last year after passing out at work 😅 turns out my ferritin was 2800... thought i was just "burned out" lol. phlebotomy every week felt like a chore but now i can actually sleep and my joints don't scream at me. also no more bronze skin 🤫 #ironisnotabronzetan
Alan Lin
January 15, 2026 AT 22:59It is imperative to underscore the profound clinical significance of early intervention in hereditary hemochromatosis. The absence of routine screening protocols within primary care frameworks represents a systemic failure of preventive medicine. Furthermore, the efficacy of therapeutic phlebotomy, while empirically validated, remains underutilized due to cognitive biases among clinicians who erroneously attribute symptoms to age or stress. This is not merely a medical oversight-it is a public health crisis.
Priyanka Kumari
January 17, 2026 AT 19:41This is such an important post! I’m a nurse in Mumbai and I’ve seen so many patients dismissed for "just being tired"-especially women after menopause. My mom was diagnosed after my dad got tested. We got the whole family screened-my sister and I both carry one copy. It’s crazy how cheap and life-saving this is. Please, if you have family history, get tested. No excuses.
Avneet Singh
January 19, 2026 AT 01:43It’s amusing how the post romanticizes phlebotomy as some kind of folk remedy. The real issue is the lack of pharmacological innovation in managing hereditary iron overload. One would expect peer-reviewed therapeutics to supersede venesection by now, yet we’re still stuck in the 19th century. The reliance on bloodletting is not just archaic-it’s a testament to the stagnation of translational medicine in genetic disorders.
Nelly Oruko
January 19, 2026 AT 16:02My dad had this. We didn’t know until he had a heart attack at 52. Now I get my ferritin checked every year. No supplements. No vitamin C with steak. And yes, I still eat red meat. But I don’t ignore the silence. It’s not about feeling good-it’s about not dying.
vishnu priyanka
January 21, 2026 AT 12:03bro i used to drink raw oysters like it was a sport 🐚💀 then i read this and now i’m scared of shellfish. also my uncle died from liver cancer at 56 and they never knew why. now i get my blood drawn like it’s a yoga class. chill but deadly serious.
Lethabo Phalafala
January 23, 2026 AT 01:06I spent 10 years being told I was "just anxious"-joint pain, fatigue, brain fog, even my skin turned gray. Then my brother got diagnosed. I got tested. Ferritin: 3,200. I had 58 phlebotomies. I lost my marriage. My kids thought I was dying. I’m not okay. But I’m alive. And if you’re reading this and you feel "off"? GET TESTED. Don’t wait until you’re a statistic.
Lance Nickie
January 23, 2026 AT 13:53phlebotomy? that’s just donating blood. why not just go to a blood bank and get paid? they’ll take your blood and you get free snacks. win win. also, iron isn’t even bad. maybe your body just needs more iron lol.
Milla Masliy
January 23, 2026 AT 14:05My mom got diagnosed after her knee replacement-doctors thought it was arthritis. Turns out it was iron poisoning. We’re Indian-American, so no one thought it was "our thing." But it’s not about race-it’s about genes. My sister and I got tested. We both carry C282Y. I started phlebotomy last month. I feel like I’ve been sleeping in a fog and someone finally opened the window.
Damario Brown
January 25, 2026 AT 05:08you people are so naive. you think phlebotomy fixes it? nah. it just hides it. the iron’s still in your cells, just moved around. and who’s to say the blood centers aren’t just profiting off your suffering? also, did you know 80% of people with hemochromatosis are misdiagnosed as having fibromyalgia? your doctor doesn’t care. they’re paid to prescribe pills, not save lives. and don’t even get me started on how the pharma industry hates this because it’s free.
sam abas
January 25, 2026 AT 12:50Okay, so let me get this straight. You’re telling me that a simple genetic mutation-C282Y homozygous-is responsible for a systemic iron overload that can lead to cirrhosis, diabetes, and cardiac arrhythmias, and yet the entire medical establishment doesn’t screen for it routinely? That’s not negligence, that’s institutional incompetence. And now you want me to believe that the solution is to bleed me weekly like some medieval cure? The real tragedy isn’t the disease-it’s that we’ve got a 21st-century genome and a 17th-century diagnostic paradigm. Also, why is there no FDA-approved hepcidin mimetic yet? Because Big Pharma doesn’t make money off blood bags. This isn’t medicine. It’s a cult.
John Pope
January 26, 2026 AT 18:39Think about this: if your body can’t regulate iron, maybe it’s not the iron that’s the problem… maybe it’s the *idea* of iron. We’ve been taught to fear deficiency, but what if excess is just nature’s way of saying: "you’re not aligned with your ancestral diet?" Maybe we’re supposed to be hunter-gatherers who burn through iron fast. Phlebotomy isn’t treatment-it’s surrender to a broken system. What if the real cure is fasting, grounding, and ancestral living? I’ve stopped phlebotomy and now I meditate with iron-rich rocks. My ferritin dropped 400 points. Coincidence? Or cosmic alignment?