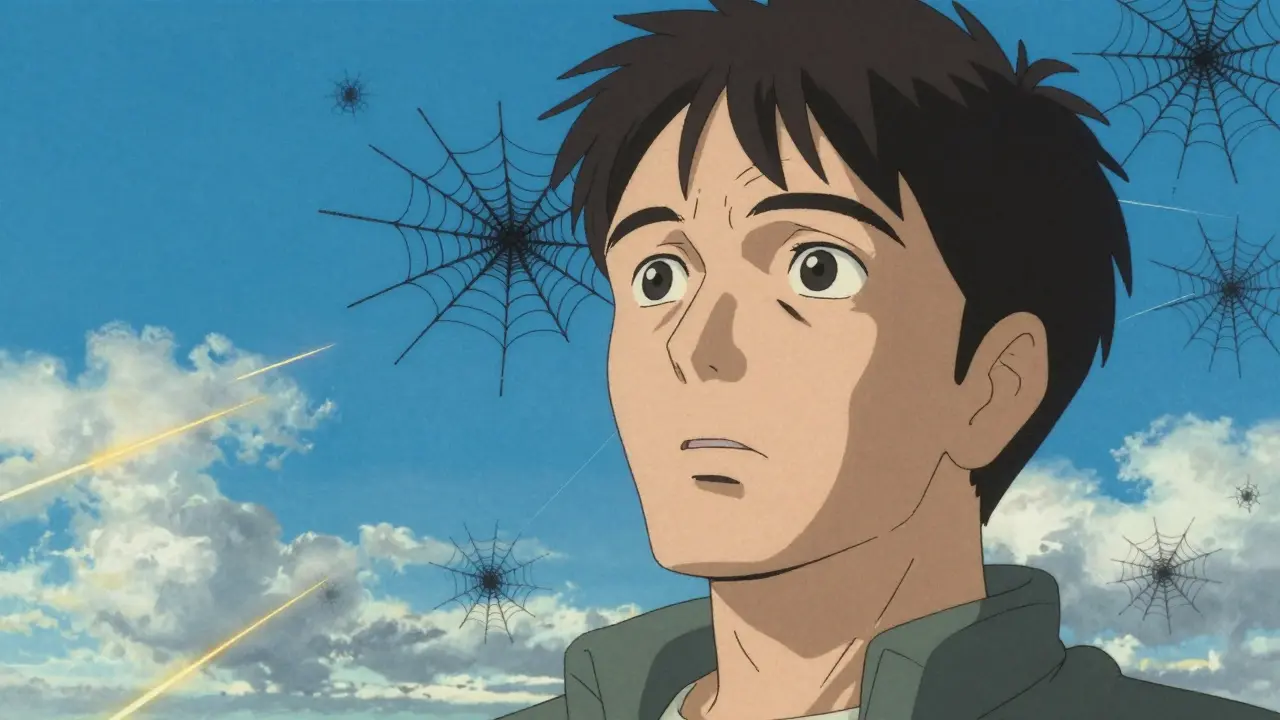
Have you ever looked up at a clear blue sky and seen tiny dots or spiderweb-like shapes drifting across your vision? Or maybe you’ve noticed sudden streaks of light in your peripheral vision, like a camera flash going off in the dark? You’re not alone. These are called floaters and flashes, and for most people over 50, they’re a normal part of aging. But sometimes, they’re a warning sign - and ignoring them could cost you your vision.
What Are Floaters and Flashes?
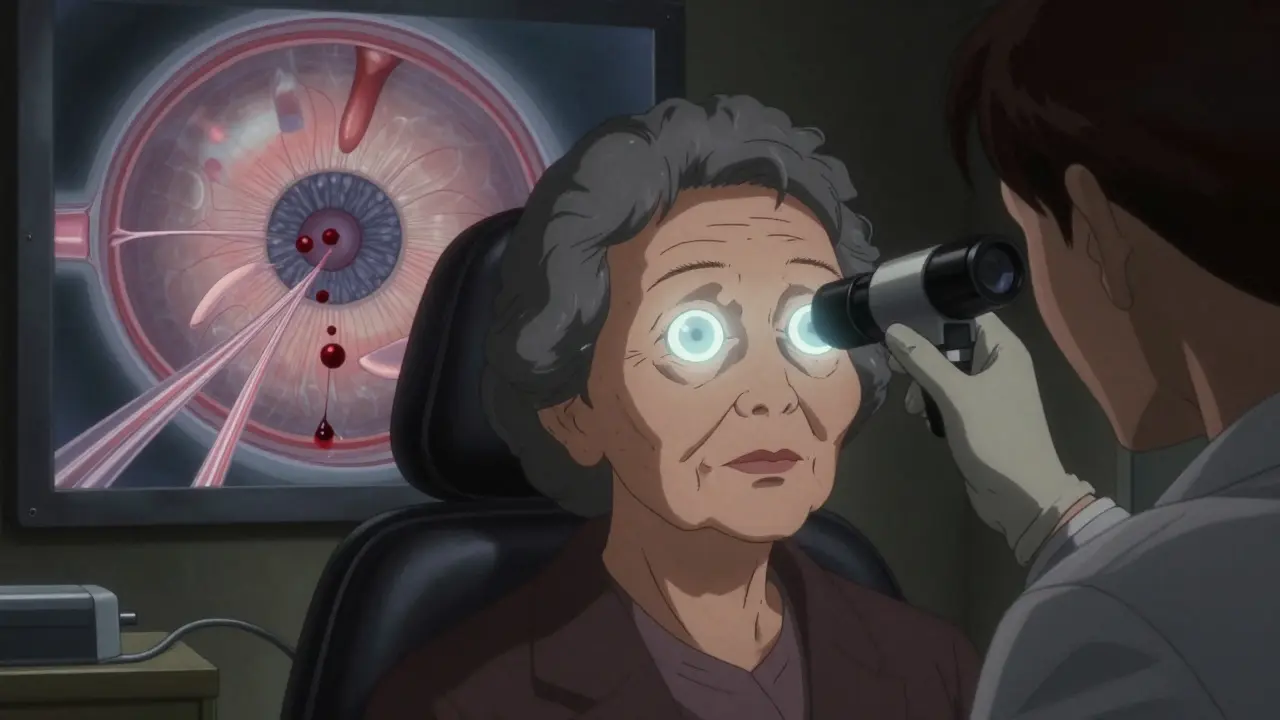
Floaters are those little shadows that seem to move when you move your eyes. They look like specks, threads, or cobwebs floating in front of your vision. They’re most noticeable against bright backgrounds - like a white wall or a clear sky. Flashes, on the other hand, are brief bursts of light you see out of the corner of your eye, often described as sparks, streaks, or lightning. They don’t come from outside your eye. They’re caused by your retina being tugged or stimulated from inside. Both happen because of changes in the vitreous - the clear, gel-like substance that fills the back two-thirds of your eye. In youth, the vitreous is thick and firm, holding the retina in place. But as you age, it starts to break down. Water separates from the collagen fibers, the gel liquefies, and slowly pulls away from the retina. This is called posterior vitreous detachment (PVD). It’s not a disease. It’s just what happens to nearly everyone over time.Why Do Floaters Appear?
As the vitreous shrinks and becomes more liquid, tiny collagen fibers clump together. These clumps cast shadows on your retina, and your brain interprets those shadows as floating objects. The more you move your eyes, the more these clumps shift around, which is why floaters seem to dart away when you try to look directly at them. Most floaters are harmless. They’re usually small, few in number, and appear gradually. People often describe them as “bubbles,” “bugs,” or “dark spots.” Over time, your brain learns to ignore them. Many find that after six months to a year, floaters are still there but no longer bother them. They settle toward the bottom of the eye, out of your direct line of sight.What Causes Flashes?
Flashes happen when the shrinking vitreous tugs on the retina. The retina is made of light-sensitive cells, and when it’s pulled, it sends a signal to your brain - even though there’s no actual light. That’s why you see flashes. They’re not hallucinations. They’re real signals from your eye. These flashes are usually brief - lasting only a second or two - and often happen in clusters. You might see several in a row over minutes or hours. They’re most common in low light or when you move your eyes quickly. Flashes often occur in one eye at a time, because the vitreous in each eye ages differently.When Is It Just Aging - and When Is It an Emergency?
The biggest risk isn’t the floaters or flashes themselves. It’s what they might be hiding. About 10-15% of people with PVD develop a retinal tear or detachment. That’s not common, but it’s serious. A retinal tear can lead to a retinal detachment - a medical emergency that can cause permanent blindness if not treated within days. Here’s how to tell the difference:- Benign PVD: You notice a few new floaters, maybe one or two flashes, and then it stops. Your vision stays clear. No dark curtain, no loss of side vision. This is the most common scenario - and it’s usually safe.
- Warning signs: Sudden shower of many new floaters, persistent flashes (especially recurring every few seconds), a dark shadow or curtain coming across your vision, sudden blurring, or loss of peripheral vision. These are red flags.
Who’s at Higher Risk?
Not everyone develops PVD at the same time. Age is the biggest factor. By age 65, about 75% of people have floaters. By 70, nearly two-thirds have had a posterior vitreous detachment. But some people are at higher risk:- People over 50 - risk increases sharply after 40.
- Nearsighted individuals - their eyes are longer, which puts more tension on the retina. They often get PVD 10-15 years earlier than people with normal vision.
- Those with diabetes - high blood sugar can damage blood vessels in the eye, leading to bleeding into the vitreous.
- People who’ve had eye surgery or trauma - even a minor injury can trigger vitreous changes.
- Anyone under 50 with new floaters or flashes - these are less likely to be normal aging and more likely to signal something serious like uveitis or retinal disease.
What Should You Do If You Notice New Symptoms?
Don’t wait. Don’t assume it’s “just aging.” If you have sudden floaters, especially if they’re accompanied by flashes or any vision loss, get your eyes checked within 24 hours. If you’re seeing repeated flashes or a dark curtain across your vision, go to an eye specialist the same day. Delaying even a few days can mean the difference between saving your vision and losing it. An eye doctor will dilate your pupils and examine your retina with a special lens. This takes about 20 minutes. It’s not painful. It’s the only way to know for sure whether you have a harmless PVD or something more dangerous. The Macular Disease Foundation Australia says it plainly: “The only way to tell whether these floaters and flashes have been caused by PVD or something else is to have your eyes examined by an optometrist or ophthalmologist.”Can You Treat Floaters?
For most people, no treatment is needed. Floaters fade over time. Your brain adapts. You learn to live with them. There are procedures - like laser vitreolysis, which uses a laser to break up large floaters - but they’re not widely recommended. The American Society of Retina Specialists says the risks (like accidentally damaging the retina) often outweigh the benefits. Plus, most insurance plans won’t cover it because it’s considered experimental. Surgery to remove the vitreous (vitrectomy) is an option for severe cases, but it’s only done when floaters are so dense they block vision entirely. It’s invasive, carries risks like cataracts or infection, and isn’t worth it for most people. So the best treatment? Patience. And regular eye checks.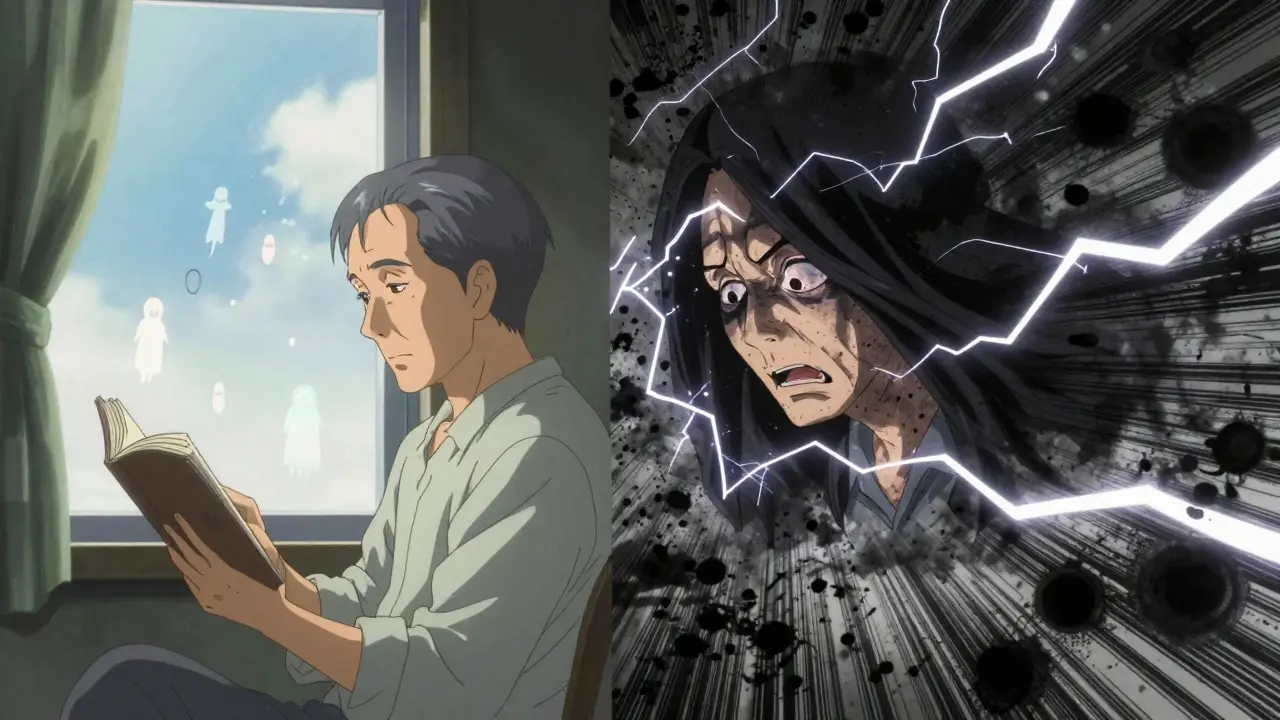
Can You Prevent Floaters and Flashes?
No. PVD is a natural part of aging. You can’t stop it. But you can reduce your risk of complications:- Control your blood sugar if you have diabetes - this prevents bleeding in the vitreous.
- Wear protective eyewear during sports or DIY projects to avoid trauma.
- Don’t ignore sudden changes. Even if you’ve had floaters before, new ones mean a new evaluation.
What Happens After Diagnosis?
If your doctor confirms it’s a simple PVD, you’ll likely be told to monitor your vision. They’ll ask you to report any new symptoms: more floaters, new flashes, or vision changes. Most people don’t need follow-up unless something changes. If they find a retinal tear, they can usually fix it in the office with laser treatment or freezing therapy. These procedures seal the tear before fluid leaks behind the retina and causes detachment. Success rates are over 90% when caught early. If it’s already a detachment, surgery is needed - and it’s more complex. Recovery takes longer. Vision may not fully return.Real Stories, Real Concerns
Many people report feeling anxious when they first notice floaters. One patient from Melbourne described it as “seeing ghosts in my vision.” Another said the flashes made her feel like she was having mini-seizures. The fear is real - and understandable. But what most people don’t know is that after their eye exam, 9 out of 10 find out it’s just PVD. Relief floods in. They learn it’s not a brain tumor, not a stroke, not something they caused. It’s just aging. One Reddit user wrote: “I thought I was going blind. Turned out it was a harmless vitreous detachment. I cried when the doctor said it was normal.”Final Advice
Floaters and flashes are common. For most, they’re harmless. But they’re also your eye’s way of whispering - sometimes shouting - that something might be wrong. If you’re over 50 and notice new floaters or flashes, don’t panic. But don’t ignore them either. Schedule an eye exam within 48 hours. If you have flashes that keep coming back, or sudden vision loss, go the same day. Your vision doesn’t come with a backup. Once the retina is damaged, there’s no undo button. But with a quick check, you can avoid disaster - and live with the floaters without fear.Are floaters and flashes always a sign of something serious?
No. Most floaters and flashes are caused by posterior vitreous detachment (PVD), a normal part of aging. About 75% of people over 65 experience them. They’re usually harmless and become less noticeable over time. But sudden changes - like a shower of new floaters, repeated flashes, or a dark curtain over your vision - can signal a retinal tear or detachment, which requires urgent care.
How long do floaters last?
Floaters from PVD typically settle within six months to a year. The brain learns to ignore them, and the debris often drifts out of your central vision. Some people may still see them occasionally, especially in bright light, but they rarely interfere with daily life. If floaters suddenly increase in number or change shape after months of stability, see your eye doctor.
Can eye drops or supplements get rid of floaters?
No. There are no eye drops, vitamins, or supplements proven to eliminate floaters. While some products claim to help, there’s no scientific evidence. The only way to remove persistent floaters is through surgery (vitrectomy), which carries significant risks and is rarely recommended unless vision is severely blocked. Patience and monitoring are the best approaches.
Why do I see floaters more in bright light?
Floaters are shadows cast by clumps of collagen in the vitreous. In bright light, your pupils shrink, letting in less peripheral light. This makes the shadows more visible against a uniform background like a white wall or blue sky. In dim light, your pupils widen, scattering light and making floaters harder to see.
Is it normal to have floaters in only one eye?
Yes. The vitreous in each eye ages independently. It’s very common to notice floaters or flashes in one eye first. If you later notice similar symptoms in the other eye, that’s also normal - it just means the vitreous in that eye is now undergoing the same age-related changes. But if one eye suddenly develops many new floaters or flashes while the other doesn’t, it’s still important to get checked.
Can stress or screen time cause floaters?
No. Stress and screen time don’t cause floaters. They may make you more aware of them - like how tension can make you notice a headache more - but they don’t create the physical changes in the vitreous. Floaters are caused by aging, nearsightedness, or eye trauma, not digital strain. Taking breaks from screens helps eye comfort, but won’t reduce floaters.
What happens if I ignore flashes and new floaters?
Ignoring sudden flashes and new floaters can be dangerous. If they’re caused by a retinal tear, fluid can leak behind the retina and cause detachment - a leading cause of preventable blindness. If treated within days, 90% of retinal detachments can be repaired successfully. If you wait weeks, the chance of permanent vision loss rises dramatically. Don’t gamble with your sight.
Terry Free
December 25, 2025 AT 11:09Let me guess-you think floaters are just ‘aging’? Newsflash: your vitreous isn’t magic, it’s physics. Collagen fibrils liquefy, posterior vitreous detachment occurs, and your retina gets tugged. It’s not ‘normal’-it’s biomechanical decay. And if you’re over 40 and not getting dilated yearly, you’re not aging, you’re gambling with your optic nerve. Stop romanticizing degeneration.
And yes, laser vitreolysis is ‘experimental’ because big pharma doesn’t profit off it. But that doesn’t mean it’s not effective. It just means you’re being sold fear instead of solutions.
Stop waiting for ‘it to fade.’ It won’t. Your brain adapts because it’s lazy, not because it’s healthy.
Get checked. Now. Or don’t. But don’t pretend ignorance is wisdom.
Sophie Stallkind
December 26, 2025 AT 00:33Thank you for this meticulously researched and clinically accurate exposition. The distinction between benign posterior vitreous detachment and the ominous heralding signs of retinal pathology is articulated with exceptional clarity. I am particularly grateful for the emphasis on timely ophthalmologic evaluation-this is not merely a suggestion, but a critical imperative in the preservation of visual integrity.
For those who may dismiss these symptoms as inconsequential, I urge a reconsideration grounded in evidence-based medicine. Vision, once compromised, is rarely restored in its entirety. Proactive care is not an indulgence; it is a moral obligation to oneself.
With profound respect for the author’s diligence in disseminating vital health information.
Michael Dillon
December 27, 2025 AT 09:46Okay but let’s be real-how many of us have stared at a white ceiling for 20 minutes just to see if the floaters ‘dance’? I swear mine do the cha-cha. And the flashes? I thought I was having tiny lightning storms in my eyeballs. Turns out it’s just my vitreous doing the tango with my retina.
Also, I’m 38 and nearsighted. I’ve had floaters since college. They’re like my personal ghosts. I don’t panic. I just blink and go about my day. If you’re not seeing a dark curtain or losing peripheral vision, chill. You’re not dying. You’re just aging. Like a fine wine. Or a slightly cloudy lens.
Also, no, screen time doesn’t cause them. I’ve been on Zoom 12 hours a day since 2020. My floaters were here before my laptop.
And yes, I Googled it. Twice. I’m fine.
Gary Hartung
December 27, 2025 AT 11:55Do you realize… that the vitreous… is not merely a gel… but a sentient, aging archive… of your entire visual history? Every blink… every tear… every midnight scroll… has left its trace… in that translucent prison… and now… it is peeling away… like the last page of a diary… written in light… and shadow…
And you… you think it’s ‘normal’? No. It is existential. It is metaphysical. It is the eye’s quiet rebellion against entropy.
And if you ignore it… you ignore the truth… that your body… is slowly… becoming… a ghost… of itself…
Go to the doctor… or… be haunted… forever.
-Gary Hartung, M.D. (in my mind)
Ben Harris
December 27, 2025 AT 12:23Jason Jasper
December 28, 2025 AT 13:36I noticed a few floaters last year after a long hike in bright sunlight. I didn’t panic. I waited a couple months. They didn’t get worse. I went to the optometrist just to be sure. Turned out it was PVD. No tear. No detachment. Just… aging.
It’s weird, but now I don’t mind them. They’re like little reminders that my body is alive, changing, adapting. I don’t fix them. I don’t fear them. I just… let them be.
But yeah-get checked if it’s sudden. No shame in that. Just don’t let fear turn a normal process into a horror story.
Mussin Machhour
December 29, 2025 AT 16:58Man, I love this post. Seriously. I thought I was going blind when I saw my first flash-I was at the gym, looked up at the ceiling lights, and BAM-lightning in my eye. Thought I was having a stroke.
Went to the doc, turned out it was just my vitreous doing its thing. Now I laugh about it. My floaters? They’re my little visual pets. I name them. There’s ‘Bob’ and ‘Squiggles.’
Don’t freak out. Get checked. Then breathe. Your eyes aren’t broken. They’re just… evolving. Like a slow-mo sci-fi movie where you’re the main character.
And no, coffee doesn’t make them worse. I’ve tried.
Justin James
December 30, 2025 AT 13:15Have you ever considered that floaters aren’t just aging? That maybe the vitreous is reacting to EMF radiation from 5G towers? That the gel is being corrupted by microplastics in our water supply? That the FDA and Big Pharma have known for decades that retinal detachment spikes correlate with fluoride in municipal water but suppressed the data because cataract surgery is a $20 billion industry?
My uncle’s neighbor’s cousin had floaters after moving near a cell tower. He went blind in six months. The doctor said ‘PVD’ but the real cause? The government’s silent war on vision.
And don’t even get me started on how blue light from screens accelerates vitreous liquefaction by 400%. That’s why kids now get floaters at 12. They’re not just looking at phones-they’re being slowly erased by invisible waves.
Wear amber glasses. Drink spring water. Avoid fluorescent lights. And if you see a flash… turn off every device. Immediately. Your retina is screaming.
Lindsay Hensel
December 31, 2025 AT 05:39Thank you for this thoughtful, compassionate guide. The balance between reassurance and urgency is masterfully struck. I have shared this with my elderly patients. Many fear the unknown-this clarifies without terrifying.
One addition: cultural stigma around aging eyes often delays care. We must normalize eye exams as routine, like dental checkups. Vision is dignity.
With gratitude.
Katherine Blumhardt
January 1, 2026 AT 19:42sagar patel
January 2, 2026 AT 13:37