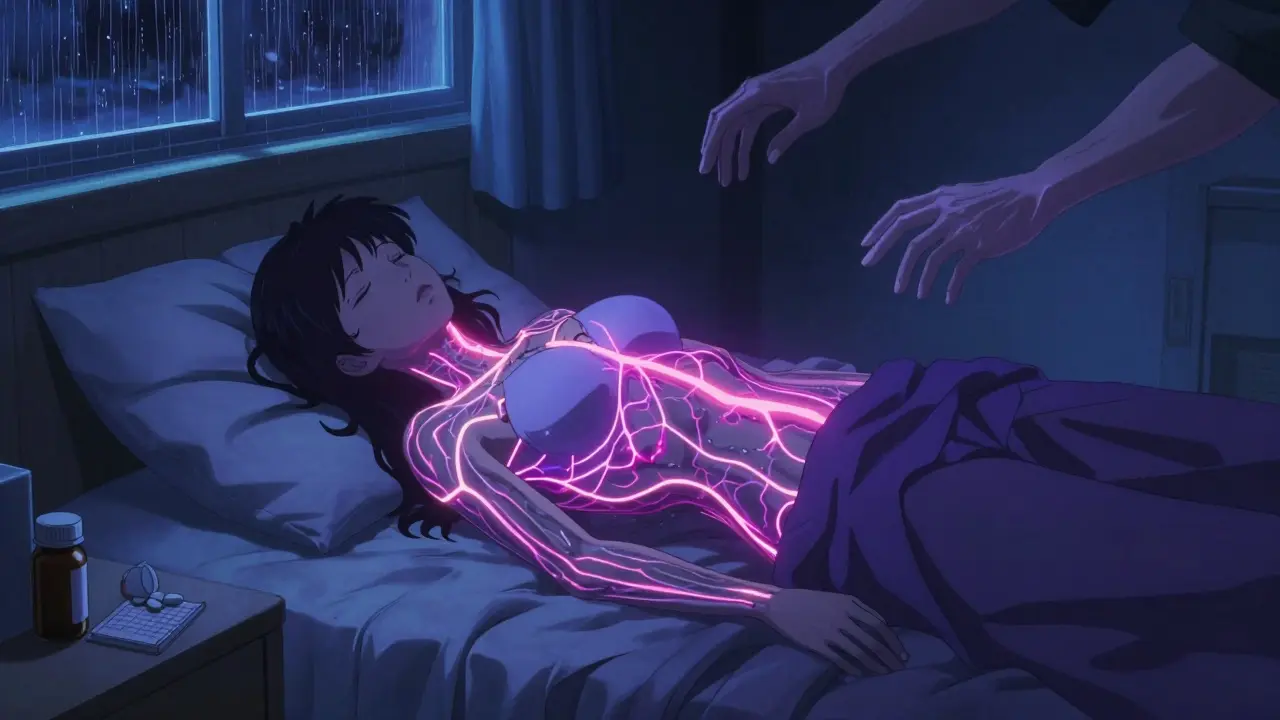
Widespread pain that doesn’t go away. Fatigue so deep it feels like your bones are heavy. Trouble remembering simple things - like where you put your keys or what you were just about to say. If this sounds familiar, you might be dealing with fibromyalgia. It’s not just "feeling tired" or "being stressed." It’s a real, measurable condition affecting the nervous system, and it’s more common than most people think. Around 2 to 8% of people worldwide have it, and in the U.S. alone, about 10 million people live with it - mostly women. Yet, many still go undiagnosed for years because the pain doesn’t show up on X-rays or blood tests. The good news? There are ways to manage it. And antidepressants, while not a cure, play a real role in helping people feel better.
What Exactly Is Fibromyalgia?
Fibromyalgia isn’t muscle damage. It’s not arthritis. It’s not a mental health disorder, even though it often comes with anxiety or depression. At its core, fibromyalgia is a disorder of how the brain and spinal cord process pain signals. People with this condition have what’s called "central sensitization" - their nervous system becomes hypersensitive. A light touch might feel painful. A quiet room might feel too loud. Even normal daily movements can trigger discomfort.
The American College of Rheumatology defines it by two main things: widespread pain lasting at least three months and at least four other symptoms like fatigue, trouble sleeping, brain fog, and mood changes. There’s no single test to confirm it. Doctors rule out other conditions - like lupus or thyroid problems - and then look for patterns. That’s why diagnosis often takes years. The average time from first symptom to diagnosis? Five years.
Why Antidepressants? You’re Not Depressed
It’s a common misconception: if you’re prescribed an antidepressant, you must be depressed. That’s not true in fibromyalgia. These medications aren’t being used to treat sadness. They’re being used to change how pain signals travel through your nerves.
Three antidepressants have FDA approval specifically for fibromyalgia:
- Duloxetine (Cymbalta) - an SNRI, usually started at 30 mg daily, then increased to 60 mg. Works in about 50% of users, with noticeable pain reduction in 4 to 6 weeks.
- Milnacipran (Savella) - another SNRI. Dosed higher, starting at 12.5 mg and building up to 100 mg daily. Similar effectiveness, but more nausea and dizziness.
- Pregabalin (Lyrica) - technically not an antidepressant, but often grouped with them. Works on nerve signals directly. Starts at 25 mg at night, can go up to 450 mg. Helps with pain and sleep, but causes dizziness in up to 40% of users.
Then there’s amitriptyline, a tricyclic antidepressant (TCA). It’s not FDA-approved for fibromyalgia, but doctors prescribe it off-label all the time - especially for sleep and pain. A low dose, like 10 mg at night, can help you sleep deeper without the next-day grogginess of higher doses. One patient from MyFibroTeam said it gave her restorative sleep after 10 years of insomnia. That kind of change can be life-shifting.
But here’s the catch: these meds don’t work for everyone. About half the people who try them don’t get meaningful relief. And side effects? They’re real. Nausea, dizziness, dry mouth, weight gain, and in some cases, increased anxiety. One survey found nearly 60% of people stopped duloxetine because of side effects. That’s why starting low and going slow is key.
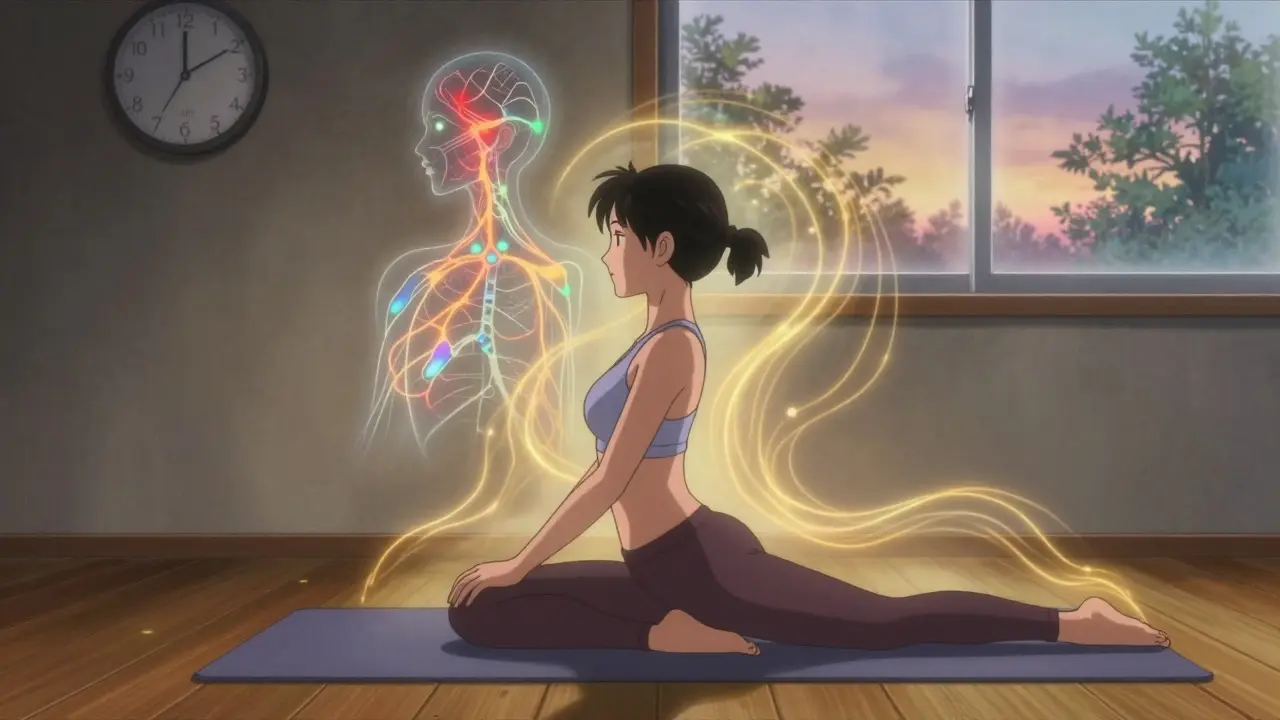
Exercise Is the Most Effective Treatment - And It’s Underused
Let’s be clear: the single most effective treatment for fibromyalgia isn’t a pill. It’s movement. But not intense workouts. Not running marathons. Gentle, consistent activity.
Studies show that regular low-impact exercise reduces pain by 25 to 35% in most people after six months. That’s better than most drugs. Tai chi, yoga, and Pilates have all been shown to help. One 2022 study found yoga reduced pain intensity by 24%. Tai chi improved pain by 20 to 30% in just 12 weeks.
The trick? Start small. Do 10 to 15 minutes a day. Walk around the block. Stretch in your living room. Slowly increase by 10% each week. Push too hard, and you’ll flare up - and that’s when people give up. The "10% rule" is the golden rule: never increase your activity level by more than 10% per week. That’s how you avoid setbacks.
And it’s not just about pain. Exercise improves sleep, lifts mood, and clears brain fog. One patient on Reddit said, "I thought I’d never feel strong again. After six months of walking and water aerobics, I carried my own groceries for the first time in years."
Cognitive Behavioral Therapy: Rewiring Your Response to Pain
When pain never leaves, your brain starts to expect it. That’s where Cognitive Behavioral Therapy (CBT) comes in. It doesn’t erase the pain. But it changes how you react to it.
CBT for fibromyalgia usually involves 8 to 12 weekly sessions, each 45 to 60 minutes long. You learn to recognize negative thought patterns - like "I’ll never get better" or "I can’t do anything" - and replace them with more helpful ones. You also learn pacing techniques: how to break tasks into smaller chunks, rest before you crash, and avoid the "boom-bust" cycle of doing too much one day and being stuck in bed the next.
Research shows CBT improves pain and function by 20 to 30%. It’s especially helpful for people who feel hopeless or overwhelmed. The problem? Access. Only about 60% of urban patients can find a therapist who specializes in chronic pain. In rural areas? It’s closer to 25%. Insurance often won’t cover it. That’s a huge barrier.
Combining Treatments: What Actually Works in Real Life
Most people don’t get better with just one thing. The best results come from stacking treatments.
A 2022 Arthritis Foundation survey of patients found that 37% of those who saw real improvement used a combination of low-dose antidepressants and gentle exercise - like 10 mg of amitriptyline at night plus three 20-minute tai chi sessions a week. Others paired duloxetine with yoga. Some added acupuncture, which studies show helps about 60% of people reduce pain by 15 to 25% after 6 to 12 sessions.
One pattern stands out: people who stick with non-drug treatments long-term do better than those who rely only on pills. Medications often help in the first few months, but their effect fades after 6 to 12 months. Exercise, CBT, and mindfulness practices? Their benefits keep growing.
Dr. Daniel Clauw from the University of Michigan says it plainly: "Exercise is the single most effective treatment for fibromyalgia, yet it’s the most underutilized." And Dr. Muhammad Hashmi at Stanford adds: "Medications should be adjuncts, not the main plan."

What Doesn’t Work - And What to Avoid
There’s a lot of noise out there. You’ll hear about miracle cures, special diets, or heavy painkillers. Here’s the truth:
- Opioids don’t work - and they’re dangerous. The CDC explicitly warns against them for fibromyalgia. They don’t reduce central pain and can make it worse over time.
- High-intensity workouts - like CrossFit or boot camps - often trigger flares. Stick to gentle, rhythmic movement.
- Detoxes and extreme diets - there’s no evidence they help fibromyalgia. Eating well matters, but you don’t need to cut out gluten or dairy unless you have a proven intolerance.
- Ignoring sleep - poor sleep makes everything worse. If you’re not sleeping, no pill will fix that. Sleep hygiene - consistent bedtime, no screens before bed, cool dark room - is non-negotiable.
Where We Are Now - And What’s Coming
The understanding of fibromyalgia has changed dramatically in the last decade. It’s no longer dismissed as "all in your head." It’s recognized as a neurological condition. That’s why research funding has doubled since 2018. The NIH just allocated $15 million to study how the brain processes pain in fibromyalgia.
On the horizon? A new drug called centanafadine (XRS-001). It showed 35% pain reduction in late-stage trials with fewer side effects than current options. It’s under FDA review as of early 2024. Also, devices like the Quell nerve stimulator - worn like a bracelet - are now FDA-cleared and helping some people reduce pain without drugs.
But the biggest shift isn’t in medicine. It’s in mindset. More doctors are now trained to treat fibromyalgia with a team approach: physical therapist, psychologist, pain specialist, and patient as the lead. That’s progress.
Getting Started: A Simple Plan
If you’ve just been diagnosed, here’s what to do next:
- Get educated - Use the CDC’s free online course "Managing Fibromyalgia" or the Fibromyalgia Collaborative Network’s "Pacing Your Day" workbook.
- Start moving - Pick one gentle activity: walking, water aerobics, or seated yoga. Do 10 minutes, 3 times a week. No more.
- Track your sleep - Use a simple journal. Note when you go to bed, when you wake up, and how rested you feel.
- Talk to your doctor about low-dose meds - If sleep is terrible, ask about 10 mg of amitriptyline at night. If pain is your main issue, ask about 30 mg of duloxetine. Start low. Go slow.
- Find support - Online groups like r/fibromyalgia or MyFibroTeam are full of people who get it. You’re not alone.
There’s no magic fix. But there’s hope. Many people with fibromyalgia go on to live full, active lives - not because the pain disappeared, but because they learned how to live with it without letting it control them.
Are antidepressants the only medication for fibromyalgia?
No. While antidepressants like duloxetine and amitriptyline are common, pregabalin (Lyrica) is also FDA-approved and works differently - targeting nerve signals directly. Other options include gabapentin and muscle relaxants, but they’re used less often. The key is that no single drug works for everyone, and they’re not meant to be used alone.
Can fibromyalgia go away on its own?
Fibromyalgia is a chronic condition, meaning it doesn’t go away completely. But symptoms can improve significantly - sometimes dramatically - with the right combination of lifestyle changes and treatments. Many people reach a point where their pain is mild and manageable, and they regain most of their daily function.
Why do some people say antidepressants made their pain worse?
Side effects vary. Some people experience increased anxiety, nausea, or dizziness - especially when starting or increasing the dose. Duloxetine, for example, can trigger anxiety attacks in sensitive individuals at higher doses. Starting at a very low dose and increasing slowly reduces this risk. If you feel worse, talk to your doctor - don’t stop abruptly.
Is fibromyalgia a mental health disorder?
No. Fibromyalgia is a neurological condition affecting how the central nervous system processes pain. While it often coexists with anxiety or depression, those are secondary effects - not the cause. The pain is real and measurable, even if it doesn’t show up on scans.
How long does it take to see results from exercise?
Most people notice small improvements in energy and sleep within 2 to 4 weeks. Pain reduction usually takes 8 to 12 weeks of consistent, gentle activity. The key is consistency - not intensity. Even short daily walks make a difference over time.
Can I stop taking antidepressants if I start exercising?
Maybe - but don’t stop on your own. Some people are able to reduce or discontinue meds after several months of consistent non-drug treatments. Others still need low doses to manage symptoms. Work with your doctor to taper safely. Stopping suddenly can cause withdrawal symptoms like dizziness, nausea, or mood swings.
Solomon Ahonsi
February 3, 2026 AT 04:28So let me get this straight - we’re prescribing antidepressants for pain like it’s some kind of magic potion? And nobody’s talking about how these things make you feel like a zombie for weeks before you even know if they work? I tried Cymbalta. Nausea, brain fog, and I still couldn’t get off the couch. Thanks for the placebo with side effects.
George Firican
February 5, 2026 AT 02:41The real tragedy here isn’t the lack of a cure - it’s the systemic failure to treat fibromyalgia as a neurological phenomenon rather than a behavioral problem masked in pharmaceuticals. We’ve reduced a complex dysregulation of central pain processing to a pill-pushing algorithm, ignoring the fact that the body’s signaling architecture is not broken, it’s overwhelmed. The nervous system isn’t malfunctioning - it’s screaming for regulation, not suppression. Exercise, mindfulness, and pacing aren’t adjuncts - they’re the foundational language of recovery, and yet we still treat them like optional hobbies. We medicate the symptom and call it progress, while the root - the chronic stress, the sleep deprivation, the emotional isolation - festers in silence.
Matt W
February 5, 2026 AT 06:38I’ve been living with this for 12 years. The antidepressants didn’t fix me - but they gave me just enough space to breathe so I could start moving again. I didn’t believe in yoga until I tried it. Now I do it every morning. It’s not about being cured. It’s about getting back the parts of your life the pain stole. You’re not weak for needing help. You’re brave for trying.
Anthony Massirman
February 5, 2026 AT 20:46Stop taking pills. Start walking. That’s it.
Eli Kiseop
February 6, 2026 AT 00:55why do they call it fibromyalgia if its not muscle pain is it just a fancy word for nervous system being glitchy
larry keenan
February 6, 2026 AT 10:56While the pharmacological interventions discussed are empirically supported in randomized controlled trials, the methodological limitations of patient-reported outcomes in fibromyalgia research remain a significant confounding variable. The heterogeneity of symptom presentation across the spectrum necessitates a stratified, personalized approach to therapeutic intervention, rather than the current one-size-fits-all model prevalent in primary care.
Akhona Myeki
February 8, 2026 AT 01:35In South Africa, we have no access to these expensive medications. We have traditional healers, fresh air, and community. You people in the West think you can buy your way out of pain with pills and therapists. We heal with rhythm, with song, with shared silence. You call it fibromyalgia - we call it the weight of the world. And we carry it without a prescription.
Chinmoy Kumar
February 8, 2026 AT 05:03i tried amitriptyline for a month and it made me so drowsy i couldnt even watch tv. i think the exercise part is real tho. i started doing 10 min of stretching every day and after 3 weeks i felt like i could actually get out of bed without crying. not a cure but its somethin
Sandeep Kumar
February 8, 2026 AT 07:22Antidepressants for pain? That’s what they teach in med school now? Lazy science. Real pain needs real medicine. Not mood stabilizers masquerading as analgesics. I’ve seen real chronic pain patients on opioids get better outcomes than these half-baked SSRIs. But sure, let’s pretend it’s all in the head while the pharma bros cash in.
Gary Mitts
February 8, 2026 AT 18:11So exercise is the cure but we still need pills to get us off the couch? Sounds like a pyramid scheme.
Murarikar Satishwar
February 10, 2026 AT 17:36Just wanted to say thank you for writing this. I was diagnosed last year and felt so alone. The part about pacing and the 10% rule changed everything for me. I used to think if I didn’t do 30 minutes of exercise, it wasn’t worth it. Now I do 8 minutes and celebrate it. My sleep improved. My brain fog lifted. I’m not cured, but I’m living again. And yes - the amitriptyline at 10mg? Night and day. Not perfect, but it gave me the bridge to get to the real work: moving, breathing, and being gentle with myself.