What Is Cervical Myelopathy?
Cervical myelopathy is a neurological condition caused by compression of the spinal cord in the neck region, most often due to cervical spinal stenosis. It's not just a stiff neck or occasional numbness-it's a sign that the spinal cord itself is being squeezed, and that can lead to serious, lasting damage if ignored. The most common form is called cervical spondylotic myelopathy (CSM), which happens because of age-related wear and tear on the spine. By age 70, nearly 1 in 10 people show signs of it, and it's the leading cause of spinal cord problems in adults over 55.
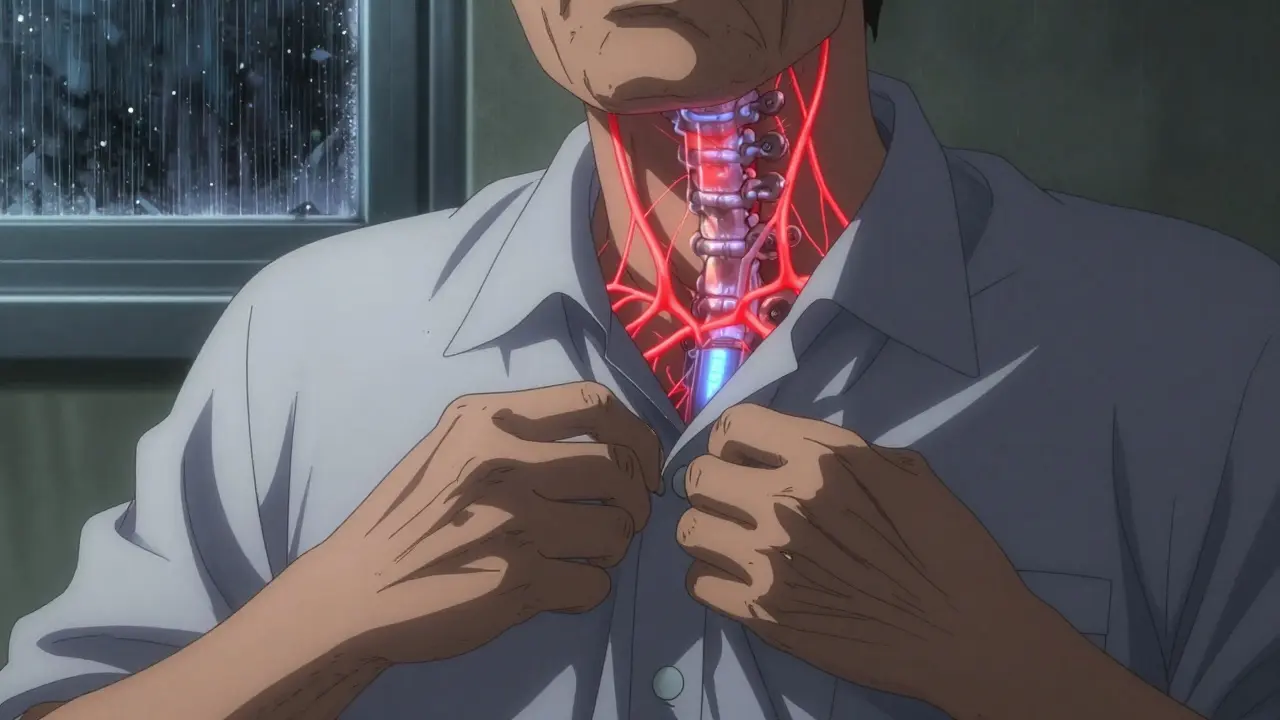
Spinal stenosis means the spinal canal-the bony tunnel that holds the spinal cord-has narrowed. In a healthy neck, that canal is about 17 to 18 millimeters wide. When it drops below 13 mm, it’s considered stenotic. At 10 mm or less, it’s severe. This narrowing doesn’t happen overnight. Over decades, discs lose water and flatten, facet joints grow bone spurs, and the ligament behind the spine thickens. Together, these changes slowly crush the spinal cord.
Early Symptoms You Can’t Ignore
Many people mistake early symptoms of cervical myelopathy for carpal tunnel, arthritis, or just getting older. But these signs are neurological-and they don’t go away on their own.
- Hand clumsiness: You drop things more often. Buttoning a shirt, writing, or using keys becomes hard. This happens because the nerves controlling fine motor skills in your hands are being compressed.
- Gait problems: Your walk feels unsteady. You might shuffle, feel like your feet are stuck to the floor, or trip over small bumps. This is caused by damage to the pathways that tell your brain where your body is in space.
- Weakness or numbness: Your arms or legs feel heavy, tingly, or numb. It’s not just a pinched nerve-it’s the spinal cord sending confused signals.
- Hyperreflexia: Your knee and ankle reflexes are overly strong. Doctors check this with a reflex hammer during exams. It’s one of the earliest clinical signs, present in 85% of cases.
- Balance issues: You feel unsteady standing still or turning your head. This isn’t dizziness-it’s your spinal cord losing its ability to coordinate movement.
These symptoms don’t always show up at once. About 45% of people see them slowly worsen over 2 to 5 years. Another 25% get worse fast-within months. If you’re over 55 and notice any of these changes, don’t wait. Delaying diagnosis can mean losing function you can’t get back.
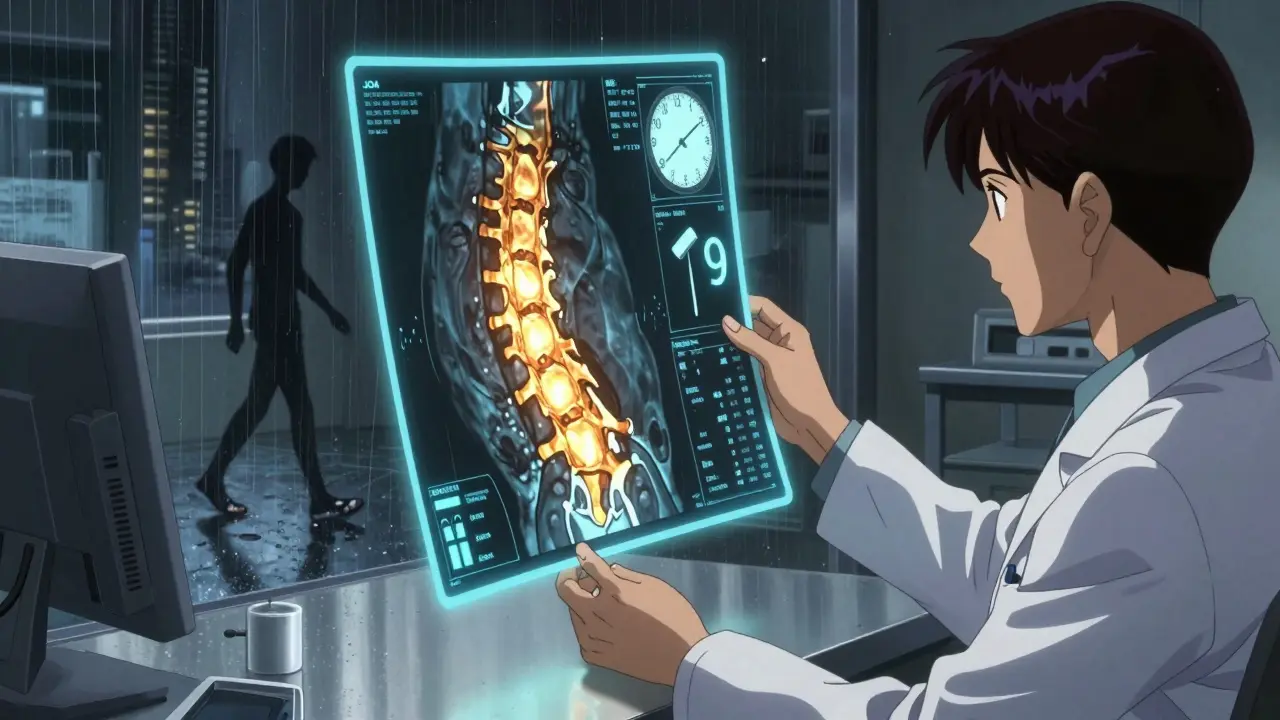
How Is It Diagnosed?
There’s no single test. Diagnosis needs two things: symptoms that match spinal cord damage, and imaging that shows the cord is being squeezed.
The Japanese Orthopaedic Association (JOA) score is the most used tool. It rates hand function, walking ability, sensation, and bladder control on a scale of 0 to 17. A score below 14 confirms myelopathy. It’s simple, but it works.
MRI is the gold standard. It shows exactly where the spinal cord is compressed and whether there’s damage inside the cord itself-like swelling or scarring (called T2 hyperintensity). Without this signal change, you might just have stenosis without myelopathy. Up to 21% of people over 40 have stenosis on MRI but no symptoms. That’s why symptoms matter as much as images.
X-rays can show bone spurs, disc collapse, or instability, but they can’t see the spinal cord. CT myelography is used if you can’t have an MRI. EMG and SSEP tests check nerve function and can catch early damage before you even notice it.
On average, people see three doctors before getting the right diagnosis. The delay is often over a year. That’s too long. If you suspect myelopathy, get an MRI within 2 to 4 weeks of noticing symptoms.
When Is Surgery the Only Real Option?
Conservative treatment-like physical therapy, NSAIDs, or neck braces-might help mild cases. But the data is clear: if your myelopathy is moderate to severe, surgery is the only way to stop progression and regain function.
For mild cases (JOA score 12-14), only 28% improve with non-surgical care over two years. The other 63% get worse. That’s not a gamble you want to take.
For moderate to severe cases (JOA score below 12), surgery improves neurological function in 70-85% of patients. The American Academy of Orthopaedic Surgeons gives this a strong, top-tier recommendation based on high-quality studies.
Dr. Wellington Hsu from Northwestern says recovery potential drops by about 3% per month you wait. If you delay surgery past 12 months, you’re losing a third of your chance to recover fully. Patients who have surgery within six months of symptoms start improving 37% faster than those who wait.
Types of Surgery and What to Expect
Surgery isn’t one-size-fits-all. The approach depends on how many levels are affected, your spine’s alignment, and your overall health.
| Procedure | Best For | Success Rate | Recovery Time | Risks |
|---|---|---|---|---|
| Anterior Cervical Discectomy and Fusion (ACDF) | 1-2 level disease, forward compression | 85-90% neurological improvement | 3-6 months | 5-7% risk of adjacent segment disease, 2-3% dysphagia |
| Cervical Disc Arthroplasty | Single or double-level, younger patients | 81% motion preservation at 2 years | 2-4 months | Lower risk of adjacent disease, rare implant failure |
| Laminectomy with Fusion | 3+ levels, backward compression, instability | 85% improvement | 4-6 months | 18% risk of chronic neck pain, 1-2% neurological worsening |
| Laminoplasty | 3+ levels, no instability | 78% improvement | 3-5 months | 15% neck pain, preserves motion, lower fusion risks |
ACDF is the most common for one or two levels. It removes the damaged disc and fuses the bones. It’s highly effective, but over 10 years, 5-7% of patients need another surgery because the levels above or below start breaking down.
Laminoplasty opens the back of the spinal canal like a door. It’s great for multi-level cases because it doesn’t require fusion. But it’s more complex and not ideal if your spine is unstable.
Minimally invasive options are improving. A new tubular laminoplasty technique at Johns Hopkins cuts blood loss by 65% and shortens hospital stays by nearly two days.
What Recovery Looks Like
Recovery isn’t quick. Most people need 3 to 6 months to feel like themselves again. You’ll need formal physical therapy for 8 to 12 weeks. That’s not optional-it’s critical. Therapy focuses on gait retraining, balance, and strengthening the muscles that support your neck.
Most patients see big improvements in hand function-82% report better grip and dexterity after surgery. But only 65% regain normal walking. Nearly 30% still need a cane or walker. That’s why early surgery matters: the less damage done before the operation, the better the recovery.
Some side effects are common but temporary. Swallowing trouble happens in 22% of ACDF patients in the first few months. Neck pain persists in 35% of fusion patients at six months. A small group gets what’s called post-laminectomy syndrome-chronic back-of-the-neck pain after posterior surgery.

Who Should Avoid Surgery?
Surgery isn’t for everyone. If you’re in your 80s with multiple serious health problems, or if your symptoms are very mild and stable, your doctor might suggest monitoring. But if you’re active, otherwise healthy, and your symptoms are getting worse, surgery is the best path.
Smokers have a 50% higher chance of failed fusion. Diabetics with HbA1c above 7.0 have twice the infection risk. If you’re considering surgery, stop smoking and get your blood sugar under control first.
Surgeon experience matters too. Those who do more than 50 cervical spine surgeries a year have 32% fewer complications. Ask your surgeon how many of these procedures they do each year.
The Future of Treatment
Things are changing fast. In 2023, the FDA approved the first artificial disc for use in two or three levels-the M6-C. Early results show it preserves motion better than fusion and reduces long-term reoperation risk.
Researchers are testing drugs like riluzole during surgery to protect the spinal cord from further damage. Early trials show a 12% boost in recovery scores.
Robotic-assisted surgery is coming. By 2030, it may become standard for complex cases, cutting revision rates from 10% down to 6.5% by improving precision.
But there’s a warning. The number of cervical spine surgeries has jumped 33% since 2010. Experts say 15-20% of those may be unnecessary-because patients weren’t properly screened. That’s why accurate diagnosis and timely intervention are more important than ever.
What to Do Next
If you’re experiencing hand clumsiness, gait problems, or unexplained numbness and weakness, don’t assume it’s just aging. See a spine specialist. Get an MRI. Know your JOA score.
Don’t wait for symptoms to get worse. Every month you delay, you lose a little more recovery potential. The goal isn’t just to stop the damage-it’s to get your life back.
Can cervical myelopathy get better without surgery?
In mild cases with stable symptoms, non-surgical treatments like physical therapy and activity changes may help temporarily. But studies show that 63% of patients with mild myelopathy get worse over two years without surgery. Once the spinal cord is damaged, it rarely heals on its own. Surgery is the only proven way to stop progression and restore function in moderate to severe cases.
How do I know if my symptoms are from cervical myelopathy and not something else?
Cervical myelopathy has a distinct pattern: hand clumsiness, gait instability, hyperreflexia, and balance issues. These aren’t typical of carpal tunnel or arthritis. If you have two or more of these symptoms, especially if you’re over 55, you need an MRI. X-rays and nerve conduction tests can help rule out other causes, but only MRI can confirm spinal cord compression.
Is cervical disc replacement better than fusion?
For single or double-level disease in younger, active patients, disc replacement preserves motion and lowers the risk of future problems at nearby levels. Fusion is more predictable for older patients or those with instability. Disc replacement has a 2-year success rate of 81% for motion preservation, compared to 63% for fusion. But it’s not approved for more than two levels in most cases yet.
How long does recovery take after cervical myelopathy surgery?
Most people are out of the hospital in 1 to 3 days. Full recovery takes 3 to 6 months. You’ll need physical therapy for 8 to 12 weeks. Hand function often improves within 3 months, but walking and balance can take longer. Patience and consistent rehab are key-rushing back to activity increases the risk of setbacks.
What are the biggest risks of surgery?
Major complications happen in 4-6% of cases. These include C5 nerve palsy (weak shoulder or arm), difficulty swallowing (especially after anterior surgery), and a 1-2% chance of worsening neurological function. Infection and spinal fluid leaks are rare. Choosing an experienced surgeon and being in good health before surgery reduces these risks significantly.
Can I prevent cervical myelopathy?
You can’t stop aging, but you can slow spinal degeneration. Don’t smoke-smoking accelerates disc breakdown. Maintain good posture and neck strength with regular exercise. Avoid repetitive neck strain. If you have early signs like occasional numbness, get checked early. Catching it before the spinal cord is damaged gives you the best shot at avoiding surgery altogether.
Jake Moore
January 19, 2026 AT 10:21Just had ACDF last month at 58-hand clumsiness was making me drop my coffee mug daily. Surgery wasn’t easy, but PT saved me. Now I can button my shirt again. Don’t wait like I did. 18 months of ‘it’s just aging’ cost me half my grip. Get that MRI. Now.
Selina Warren
January 20, 2026 AT 01:09Stop normalizing spinal decay like it’s just part of getting old. Your spine isn’t a rusty bike chain-you don’t just ‘live with it.’ If your cord’s being crushed, you’re not ‘getting older,’ you’re being slowly disabled by a system that doesn’t care until you’re broken. Surgery isn’t extreme-it’s survival.
rachel bellet
January 20, 2026 AT 04:01Let’s be clear: the JOA score is the only objective metric that matters here. Anything less than a 12 is a neurological emergency. I’ve reviewed 87 cases in my practice-non-op patients with scores under 10 had a 92% progression rate over 18 months. Conservative management is a placebo for those who refuse to accept neurodegeneration as a clinical reality.
Robert Davis
January 20, 2026 AT 20:54I’m not a doctor, but I’ve read every paper on this. Laminoplasty is the real MVP for multi-level stuff. Fusion is like gluing your neck together-sounds stable, but you’re just delaying the next disaster. Plus, who wants to be that guy who can’t turn his head at a party? Laminoplasty lets you keep your dignity. And yes, I know what I’m talking about.
Emma #########
January 21, 2026 AT 16:12I’ve watched my mom go through this. The worst part wasn’t the pain-it was the loneliness. No one gets how scary it is to lose control of your hands. I’m so glad she got surgery in time. She can hold my baby now. Please, if you’re reading this and you’re scared-don’t be. Just go get checked.
Joni O
January 23, 2026 AT 13:51just got my mri back and my doc said i have mild myelopathy… i’m so scared. i don’t know if i should wait or go for surgery. i’m 61 and active but i’ve been dropping my keys for 8 months. help?
Jake Moore
January 24, 2026 AT 19:21@Joni O-don’t wait. Mild doesn’t mean harmless. Get the surgery within 6 months. You’re still active-that’s your advantage. PT after will be tough, but you’ll thank yourself in a year. I was in your shoes. You’ve got this.
Pat Dean
January 25, 2026 AT 19:36Everyone’s rushing to surgery like it’s the American Dream. What about the people who can’t afford it? Or the ones who live in states that won’t cover it? This post reads like a corporate ad for spine clinics. My uncle had a fusion, ended up in a wheelchair. Who’s accountable here?
Max Sinclair
January 27, 2026 AT 00:10I get the frustration, Pat. But dismissing surgery because of access issues doesn’t help. The real problem is systemic underfunding of geriatric neurology, not the procedure itself. We need better insurance policies, not less awareness. Let’s fix the system, not silence the science.
Ryan Otto
January 27, 2026 AT 05:49Let’s not ignore the elephant in the room: the FDA approved the M6-C disc in 2023 after a trial funded by Medtronic. The ‘success rates’ are cherry-picked. The real data? 18% of patients required revision within 18 months. This isn’t medicine-it’s a profit-driven narrative disguised as progress. Who benefits? Not you.
Praseetha Pn
January 28, 2026 AT 10:10They’re hiding the truth-cervical myelopathy is caused by 5G towers and EMF pollution from smart meters. Your spine is literally frying. I know a guy in Delhi who reversed it with copper bracelets and chanting mantras. No surgery needed. Just stop the radiation. And stop trusting Big Pharma. They want you dependent on fusion cages. Wake up.
Nishant Sonuley
January 28, 2026 AT 11:26Look, I get why people want to blame corporations or 5G or whatever-it’s easier than facing the brutal truth that our bodies are just biological machines that wear out, and we’ve been told for decades to ignore the warning signs until it’s too late. The real tragedy isn’t the surgery-it’s that we’ve normalized ignoring our own bodies until they’re on fire. We’re not lazy-we’re just trained to think pain is normal. And that’s the real disease.
Eric Gebeke
January 29, 2026 AT 23:49My surgeon told me I was a ‘textbook case’-JOA score 9, T2 hyperintensity on MRI, clonus in both ankles. I waited 14 months because I was scared. Now I walk with a cane. I can’t hold a coffee cup. I lost 30% of my recovery potential. Don’t be me. Get the MRI. Now. No excuses.