Antiplatelet Drug Selector Tool
Personalized Antiplatelet Recommendation
This tool helps you understand which antiplatelet drug might be most appropriate for your situation based on the latest medical guidelines and your specific health factors.
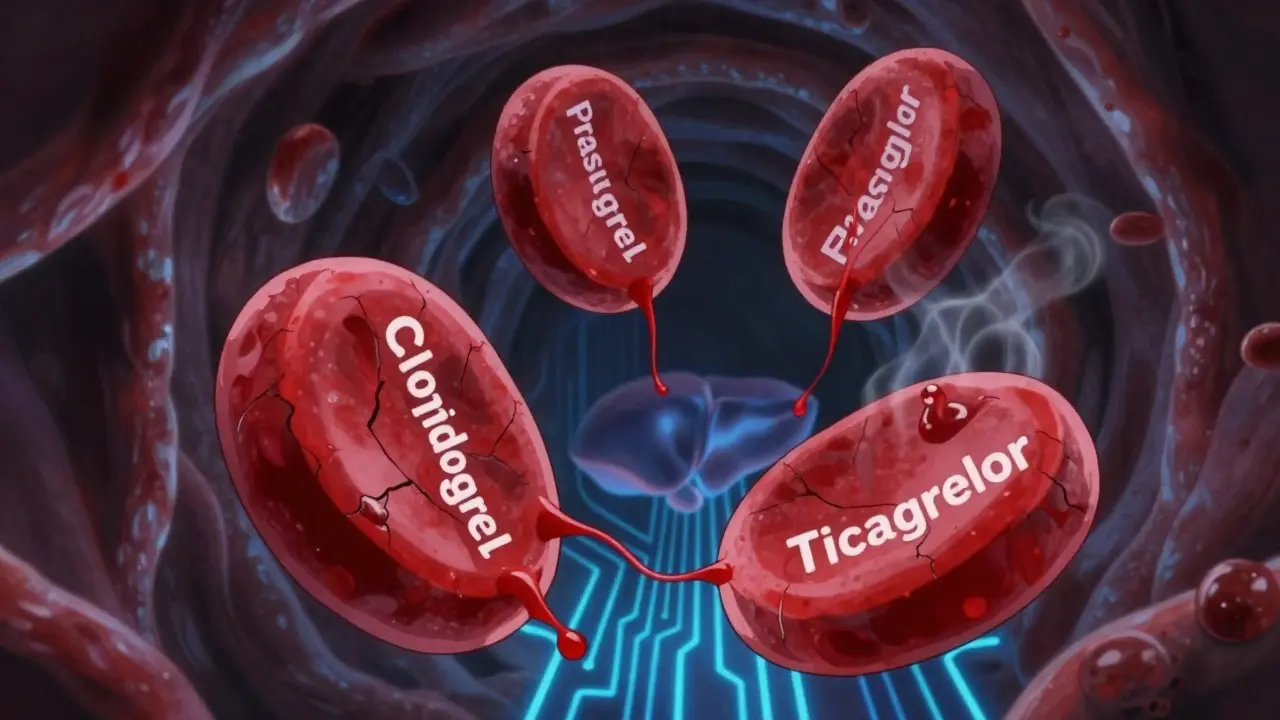
When you’ve had a heart attack or a stent placed, your doctor gives you a blood thinner-not to thin your blood like water, but to stop platelets from clumping together and forming dangerous clots. Three drugs dominate this space: clopidogrel, prasugrel, and ticagrelor. They all block the same receptor on platelets, but their side effects? They’re not the same. Choosing the right one isn’t about which is strongest-it’s about which fits your body, your risks, and your life.
How These Drugs Work (And Why It Matters)
All three are P2Y12 inhibitors. That means they block a signal on platelets that says, "Stick together!" Without that signal, clots form slower. But here’s the catch: they don’t all work the same way.Clopidogrel and prasugrel are prodrugs. Your liver has to turn them into their active form. If your liver doesn’t process them well-because of your genes-you might not get enough protection. About 1 in 3 people have a genetic variation (CYP2C19 loss-of-function) that makes clopidogrel less effective. That’s not a small number. It’s why some people still have clots even though they’re taking their pill.
Ticagrelor doesn’t need that step. It works right away, no liver conversion needed. That’s why it’s more consistent. But it also means it hits harder and faster-and that changes the side effect profile.
The Big Risk: Bleeding
All three drugs increase your risk of bleeding. That’s the trade-off. No clotting means no heart attack-but it also means if you cut yourself, you bleed longer. If you fall, you bruise harder. If something goes wrong inside, it can get dangerous.Prasugrel has the highest bleeding risk. In the TRITON-TIMI 38 trial, patients on prasugrel had 2.4% major bleeding compared to 1.8% on clopidogrel. That might sound small, but it’s enough to send people to the ER. And fatal bleeding? 0.4% vs 0.1%. That’s four times higher. That’s why prasugrel is avoided in people over 75, under 60 kg, or with a past stroke.
Ticagrelor’s bleeding risk is slightly higher than clopidogrel-2.6% vs 2.3% in the PLATO trial. Not a huge gap, but enough to matter. And here’s what most people don’t realize: ticagrelor increases bleeding that doesn’t come from surgery. Think nosebleeds, bloody stools, brain bleeds. It’s not just about big injuries.
Clopidogrel is the safest in this group for bleeding, but only if your body actually activates it. If you’re a poor metabolizer, your bleeding risk might be low-but so is your protection. You’re getting the safety without the benefit.
Ticagrelor’s Hidden Side Effect: Trouble Breathing
This one catches people off guard. About 1 in 7 people on ticagrelor start feeling like they can’t catch their breath. It’s not anxiety. It’s not asthma. It’s a direct effect of the drug. In the PLATO trial, 14-16% of patients reported dyspnea compared to 8-10% on placebo.It usually shows up in the first week. Feels like you just ran a mile when you haven’t moved. Some describe it as "drowning in air." It’s not life-threatening, but it’s terrifying. And it’s why 15-20% of patients stop taking it.
Here’s the good news: if you’re warned ahead of time, most people stick with it. Studies show 60-70% continue after being told, "This is normal, it’ll pass." But if you’re not warned? You might quit-and put yourself at risk for a clot.

Other Side Effects You Can’t Ignore
Ticagrelor also causes brief heart pauses-3.1% of people have them, compared to 2% on clopidogrel. These aren’t heart attacks. They’re short stops in the heartbeat you won’t even feel. But if you have a pacemaker or a history of slow heart rhythms, your doctor needs to know.Prasugrel’s biggest problem isn’t just bleeding-it’s how much it increases risk in certain groups. If you’re 80, weigh 55 kg, and have high blood pressure, prasugrel can drop your hemoglobin from 12 to 8 in days. That’s a blood transfusion waiting to happen.
Clopidogrel’s issue is unpredictability. You might take it for years and never have a clot. Or you might have one the day after your stent. There’s no way to know unless you get a genetic test-which costs $200-$300 and isn’t routinely done.
Dosing, Timing, and Surgery
These drugs don’t just differ in side effects-they differ in how you stop them.If you need surgery, you have to stop them first. Stop clopidogrel 5 days before. Stop prasugrel 7 days before. Stop ticagrelor just 3 days before. That’s huge for planning. If you’re scheduled for knee replacement in two weeks, ticagrelor gives you more flexibility.
Also, ticagrelor is taken twice a day. Prasugrel and clopidogrel are once a day. That’s one more pill, one more time to forget. And if you miss a dose? Ticagrelor’s effect fades faster. That’s why adherence matters more.
Who Gets Which Drug?
Guidelines are clear, but real life is messy.For someone under 75, no past stroke, and a high risk of another heart attack? Prasugrel is the strongest shield. But if they’re frail, small, or have a history of ulcers? Too risky.
Ticagrelor is now the top pick for almost all acute heart attack patients-regardless of whether they get a stent. Why? It cuts death from heart disease by 1.4 percentage points compared to clopidogrel. That’s not small. But if they’re a runner, a swimmer, or someone who’s active? The breathing trouble might ruin their quality of life.
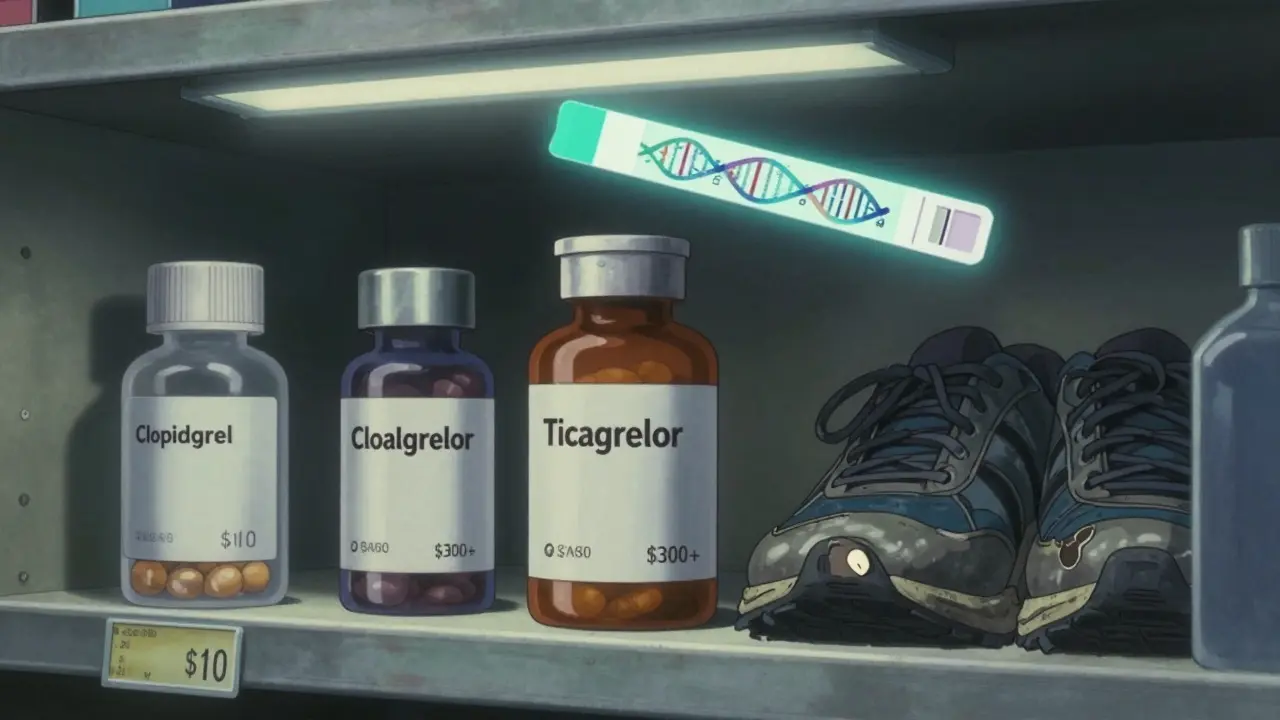
Clopidogrel? Still used in 60% of cases-not because it’s best, but because it’s cheap. Generic clopidogrel costs about $10 a month. Ticagrelor and prasugrel? $300-$400. Insurance might cover it, but copays can be brutal. Many patients choose clopidogrel because they can’t afford the others-even if it’s less effective for them.
What’s New in 2026?
In 2023, the FDA approved a lower dose of ticagrelor: 60 mg twice daily instead of 90 mg. The MATTERHORN trial showed this cut bleeding by 25% while keeping the same protection against heart attacks. That’s a game-changer for long-term use.Now, after 6-12 months of full-dose therapy, many patients switch to low-dose ticagrelor plus aspirin. It’s a smarter balance: keep the protection, reduce the side effects.
Researchers are also testing new drugs like selatogrel-a subcutaneous injection that works fast and wears off fast. Imagine being able to turn off your blood thinner before surgery with a shot. That’s the future.
What Should You Do?
If you’re on one of these drugs:- Don’t stop it without talking to your doctor-even if you feel fine.
- If you notice new shortness of breath on ticagrelor, tell your doctor. Don’t assume it’s anxiety.
- If you bruise easily, have black stools, or get headaches with vomiting, get checked immediately.
- Ask if you’re a candidate for genetic testing if you’ve had a clot despite taking clopidogrel.
- Know your bleeding risk: age, weight, kidney function, past bleeding, other meds like NSAIDs.
There’s no perfect drug. Only the right one-for you.
Which antiplatelet drug has the least bleeding risk?
Clopidogrel has the lowest bleeding risk among the three, but only if your body metabolizes it properly. About 30% of people-especially those with CYP2C19 gene variants-don’t get enough protection from clopidogrel, so their real risk of clotting may be higher than their bleeding risk. For those who respond well, clopidogrel is the safest in terms of bleeding, but not necessarily the safest overall.
Why does ticagrelor cause shortness of breath?
Ticagrelor blocks a receptor in the lungs that helps regulate breathing signals. This causes a sensation of breathlessness, even when oxygen levels are normal. It’s not asthma or heart failure-it’s a direct drug effect. The exact mechanism isn’t fully understood, but it’s reversible and often improves over time. About 1 in 7 patients experience it, and it’s the most common reason people stop taking ticagrelor.
Can I switch from clopidogrel to ticagrelor if I’m still having clots?
Yes, if you’ve had a clot despite taking clopidogrel, switching to ticagrelor or prasugrel is a standard recommendation. Clopidogrel’s variable effectiveness makes it unreliable for high-risk patients. Ticagrelor, which doesn’t need liver activation, offers more consistent platelet inhibition. Studies show switching reduces the risk of another heart attack by about 20% in these cases.
Is prasugrel safe for elderly patients?
Generally, no. Prasugrel is not recommended for patients over 75 years old or those weighing less than 60 kg. In these groups, the risk of severe or fatal bleeding rises sharply. Clinical trials showed bleeding rates nearly doubled in elderly patients on prasugrel compared to clopidogrel. For older adults, ticagrelor or low-dose clopidogrel (if genetically responsive) are safer choices.
How long before surgery should I stop each drug?
Stop clopidogrel 5 days before surgery, prasugrel 7 days before, and ticagrelor 3 days before. These are based on how long each drug’s effect lasts in the body. Stopping too early increases clot risk; stopping too late increases bleeding risk. Always confirm with your surgeon and cardiologist-they’ll consider your specific condition and the type of surgery.
Can I take ibuprofen or aspirin with these drugs?
Aspirin is usually taken with these drugs as part of dual therapy, but only in low doses (75-100 mg). Ibuprofen and other NSAIDs (like naproxen or celecoxib) increase bleeding risk and should be avoided unless absolutely necessary. If you need pain relief, acetaminophen (paracetamol) is the safest option. Always check with your doctor before taking any new medication.
Are there cheaper alternatives to ticagrelor and prasugrel?
Clopidogrel is the only generic option and costs about $10 a month. Ticagrelor and prasugrel are brand-only and cost $300-$400 per month. While clopidogrel is cheaper, it’s not always as effective. Some patients qualify for patient assistance programs from manufacturers to reduce costs. Insurance often covers ticagrelor or prasugrel if clopidogrel failed or isn’t suitable.
Cheryl Griffith
January 18, 2026 AT 03:46I had ticagrelor after my stent and the shortness of breath nearly made me quit. I thought I was having a panic attack until my cardiologist said, 'That's the drug.' Once I knew it wasn't my heart failing, I stuck with it. It’s weird, but it fades. Don’t panic-just call your doc.
Kasey Summerer
January 19, 2026 AT 09:01So let me get this straight… we’re giving people a drug that makes them feel like they’re drowning in air… but it saves lives? 🤦♂️
Isabella Reid
January 21, 2026 AT 07:37My mom switched from clopidogrel to ticagrelor after a mini-clot. She’s 72, weighs 110 lbs, and now she’s got this weird breathless feeling-but she’s alive. We didn’t know about the genetic testing until after the fact. If your doc doesn’t mention it, ask. It’s not expensive, and it could save your life.
Nicholas Gabriel
January 21, 2026 AT 18:22Let me be very clear: clopidogrel is not a 'safe' option for everyone-it’s a gamble. If you’re a poor metabolizer (and you don’t know if you are), you’re essentially taking a sugar pill with bleeding risk. Genetic testing isn’t optional if you’ve had a stent. It’s basic science. Why are we still treating this like a coin flip in 2026?
And for the love of all that’s holy, stop giving prasugrel to elderly patients who weigh less than 60 kg. I’ve seen three patients in my practice bleed out because someone thought 'stronger drug = better.' No. It’s not better. It’s lethal.
Ticagrelor’s dyspnea? Real. Not anxiety. Not deconditioning. It’s the drug. And yes, 15-20% quit. But if you warn them upfront? 70% stick with it. That’s not a side effect-it’s a communication failure.
And yes, the 60 mg dose is a game-changer. I’ve been switching my stable patients to it after 12 months. Bleeding drops. Protection stays. Why wasn’t this the standard from day one?
Also, ibuprofen? No. Just no. Acetaminophen is your friend. NSAIDs are the silent killer here. And yes, I’m yelling at you, Dr. Google, who told your cousin to take Advil for her headache while on ticagrelor.
Jody Fahrenkrug
January 23, 2026 AT 05:08I’ve been on clopidogrel for 4 years. No issues. But I also don’t know if my liver handles it well. Should I get tested? It’s $250… and my insurance says no.
Allen Davidson
January 23, 2026 AT 21:47My brother took prasugrel after his heart attack. He’s 68, 5’7”, 145 lbs. They told him it was the best. Two weeks later, he was in the ER with a GI bleed. They didn’t even check his weight. He’s fine now, but he’s on ticagrelor. If your doc doesn’t ask your weight, find a new one.
Corey Sawchuk
January 24, 2026 AT 09:19My dad switched to low-dose ticagrelor after 12 months. He’s 78. The breathlessness is gone, his hemoglobin’s stable, and he’s still alive. This is the future right here.
swarnima singh
January 25, 2026 AT 03:12why do we even need these drugs? like… isnt life supposed to be natural? i mean… we used to live without pills… now we need 7 different ones just to not die from our own blood? 🤔
Henry Ip
January 25, 2026 AT 20:07My wife is on ticagrelor. She’s a yoga instructor. The dyspnea scared her at first. We told her it’s normal. She kept going. Now she says it’s like her lungs are just… more aware. Weird, but not bad. Don’t stop without talking to your doctor.
Isabella Reid
January 26, 2026 AT 07:37Just read the comment above about yoga and dyspnea. That’s exactly why we need better patient education. Not everyone’s going to Google this. We need pamphlets. Videos. Doctors who actually explain it.
vivek kumar
January 27, 2026 AT 09:09There’s a new drug in phase 3 trials called selatogrel-it’s injected under the skin, works in 15 minutes, and wears off in 4 hours. Imagine being able to pause your anticoagulation before surgery like flipping a switch. This is the next decade.
Christina Bilotti
January 28, 2026 AT 02:11Of course clopidogrel is still used in 60% of cases. Most doctors are lazy. They don’t want to order genetic tests. They don’t want to explain dyspnea. They just want to hand out the cheapest pill and move on. And patients? They’re too tired to fight. This isn’t medicine. It’s triage.