Side Effect Management Calculator
Symptom Management Estimator
Estimate your side effect improvement timeline based on the article's clinical data and management strategies
When you're managing Type 2 diabetes, the goal isn't just to lower your blood sugar-it's to do it without making your life harder. That’s where alpha-glucosidase inhibitors come in. These drugs, like acarbose and miglitol, are designed to blunt the spike in blood sugar after meals by slowing down how fast your body breaks down carbs. Sounds smart, right? But for many people, the trade-off is rough: constant gas, bloating, and sometimes diarrhea. If you’ve been prescribed one of these medications and are wondering why you feel like a pressure cooker after lunch, you’re not alone.
How Alpha-Glucosidase Inhibitors Actually Work
These drugs don’t get absorbed into your bloodstream like most diabetes meds. Instead, they stay right where they’re needed-in your small intestine. There, they block the enzymes (alpha-glucosidases) that normally chop up complex carbs like bread, pasta, and potatoes into simple sugars your body can absorb. So instead of sugar flooding into your blood after a meal, it moves slowly, or even gets passed along undigested to your colon.
This is why they’re good for controlling post-meal spikes. Studies show they can drop postprandial glucose by 40-50 mg/dL on average. And unlike sulfonylureas or insulin, they don’t cause low blood sugar on their own. They also don’t make you gain weight, which is a big plus if you’re overweight or obese. That’s why doctors still reach for them-especially for older adults or people with kidney issues who can’t use other drugs safely.
Why Gas, Bloating, and Diarrhea Happen
Here’s the catch: the carbs that aren’t broken down in the small intestine don’t just disappear. They head straight to your colon, where your gut bacteria feast on them. That fermentation process produces gas-lots of it. And when those undigested carbs pull water into your colon, it leads to loose stools or diarrhea.
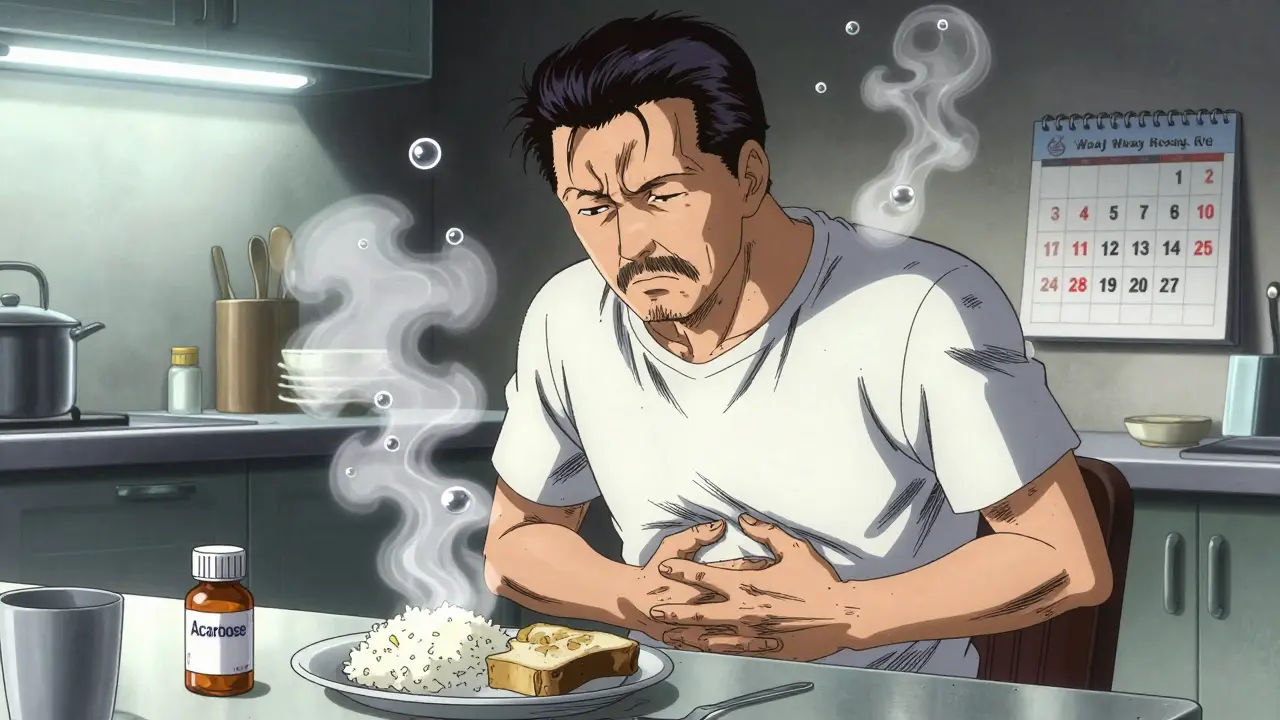
The numbers don’t lie. Clinical trials show 30-50% of people on acarbose or miglitol get flatulence. Up to 73% report it in the first month. Abdominal discomfort affects 14-30%, and diarrhea hits 10-20%. These aren’t rare side effects-they’re the norm, especially when you start.
And unlike metformin, which usually causes nausea or stomach upset, these drugs target your lower GI tract. That’s why you feel bloated, gassy, and maybe have to rush to the bathroom-not because you ate something bad, but because your body’s digestion got interrupted on purpose.
Real People, Real Reactions
Online forums are full of stories like this: a Reddit user started acarbose at 50 mg three times a day and quit after two weeks because the gas was unbearable. Another person on HealthUnlocked said they went from four bowel movements a week to almost daily, with bloating so bad their clothes felt tight.
But not everyone gives up. Some users report the same symptoms in the first month, then notice a big improvement by month three. One Drugs.com reviewer wrote: "The first month was rough. By month three, it was manageable-and my after-meal sugars dropped from 220 to 160 consistently." The key difference? Patience and strategy.
How to Reduce the Side Effects
There’s no magic pill to make these side effects vanish overnight. But there are proven ways to make them bearable-and keep you on the medication long enough to see the benefits.
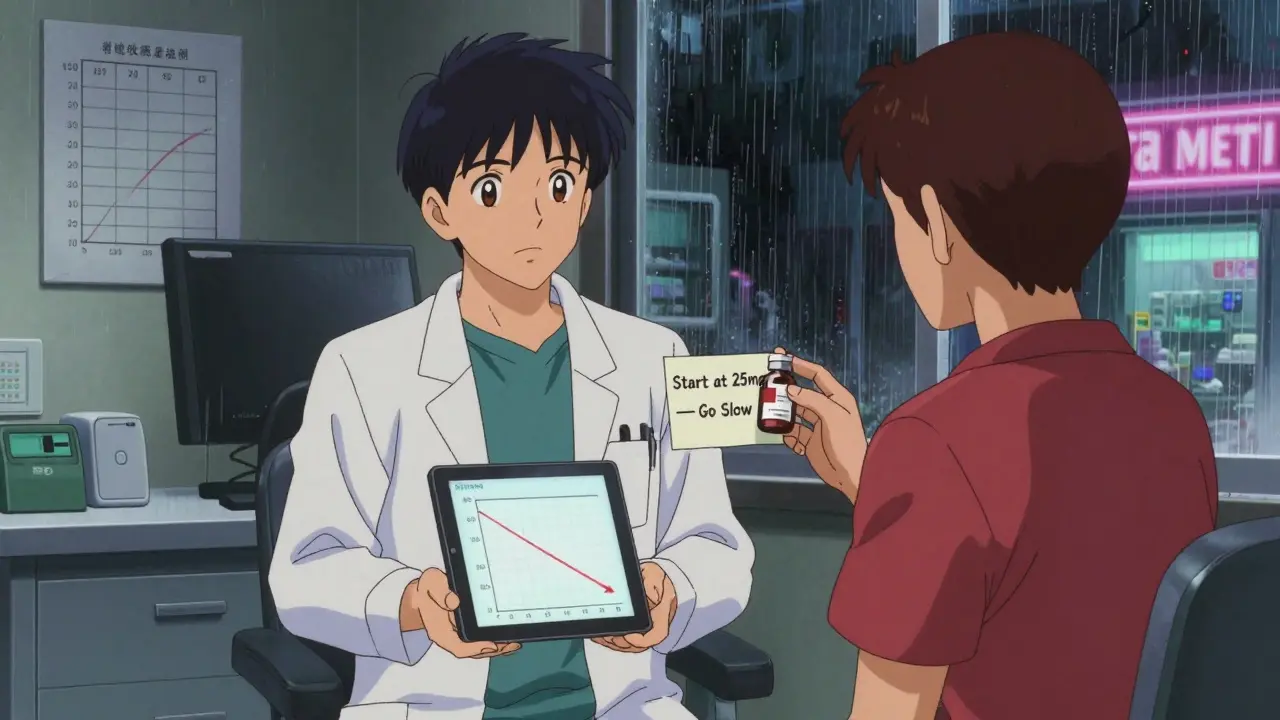
- Start low, go slow. Don’t jump to 50 mg or 100 mg right away. Begin with 25 mg once a day with your biggest meal. Wait two weeks. Then add a second dose. Then a third. This gives your gut time to adjust.
- Adjust your diet. You don’t have to go keto, but you do need to cut back on fast-digesting carbs: white bread, rice, potatoes, sugary snacks, and fruit juices. Swap them for whole grains, legumes, and vegetables with fiber. Aim for 30-45 grams of carbs per meal. A 2022 patient survey found that those who made these changes were twice as likely to stick with the drug.
- Avoid Beano. It sounds like a good idea-it’s an enzyme that helps break down beans and veggies. But it contains alpha-galactosidase, which directly conflicts with acarbose. Using both can cancel out the drug’s effect and make symptoms worse.
- Try simethicone. If gas is your main issue, taking simethicone (like Gas-X or Mylanta Gas) 15 minutes before meals can help break up bubbles. It won’t stop the gas from forming, but it can make it less painful.
- Use loperamide sparingly. If diarrhea becomes a problem, Imodium A-D (2 mg) can help. But don’t rely on it daily. It masks the problem, doesn’t fix it. And avoid high-fat meals-they make diarrhea worse.
When to Consider Stopping
Not everyone can tolerate these side effects. About 15-20% of people quit within the first three months. That’s a high dropout rate. But here’s the thing: if you’ve tried the strategies above and still can’t function normally, it’s okay to stop.
There are better options now. GLP-1 agonists like semaglutide lower blood sugar more effectively and even help with weight loss. SGLT2 inhibitors reduce heart and kidney risks. But they’re expensive. If cost is an issue, and you’re not a candidate for those drugs, acarbose still has value-especially if you’re over 65, have kidney disease, or want to avoid hypoglycemia.
Some doctors now reserve these drugs for prediabetes or as a last-line add-on. But they’re not obsolete. In countries like China and India, where diets are high in rice and wheat, alpha-glucosidase inhibitors are still widely used. Their low cost-$15 to $25 a month for generic acarbose-makes them practical in places where newer drugs aren’t accessible.
What Experts Say
Dr. John B. Buse, past president of the American Diabetes Association, says the biggest barrier to using these drugs isn’t effectiveness-it’s tolerability. But he adds: "Proper education and slow titration can make a huge difference."
The Endocrine Society’s 2023 guidelines still list them as a second- or third-line option-not because they don’t work, but because they’re hard to live with. Dr. Robert A. Rizza from Mayo Clinic puts it bluntly: "Start at 25 mg. Go slow. Tell patients it gets better in 8 to 12 weeks. Most of them don’t know that."
Meanwhile, new research is looking at combining acarbose with specific probiotics. A 2023 trial showed a 35% drop in gas severity when patients took Lactobacillus acidophilus and Bifidobacterium lactis alongside the drug. It’s early, but it’s promising.
Bottom Line: Is It Worth It?
Alpha-glucosidase inhibitors work. They lower your blood sugar after meals. They don’t cause low blood sugar. They don’t make you gain weight. And they’re cheap.
But they come with a cost: your comfort. If you’re willing to stick with the first few tough weeks, tweak your diet, and take it slow, many people find relief-and better control-within three months. If you’re not, there are other options.
Don’t let fear of gas keep you from talking to your doctor. But don’t suffer in silence either. Ask about the steps above. Ask about alternatives. And if you do keep taking it, remember: the worst of it usually passes. Your gut adapts. Your blood sugar improves. And if you can handle the discomfort, you might just find a tool that fits your life better than you expected.
Do alpha-glucosidase inhibitors cause weight gain?
No. Unlike insulin or some other diabetes drugs, alpha-glucosidase inhibitors like acarbose and miglitol don’t cause weight gain. In fact, because they reduce the amount of sugar your body absorbs from meals, some people even lose a small amount of weight. This makes them a good option for people with Type 2 diabetes who are overweight or obese.
Can I take Beano with acarbose?
No. Beano contains alpha-galactosidase, an enzyme that breaks down complex carbs in the small intestine. Since acarbose works by blocking those same enzymes, taking Beano at the same time cancels out acarbose’s effect. You might get less gas, but your blood sugar won’t be controlled. Stick to simethicone for gas relief instead.
How long do the side effects last?
For most people, gas, bloating, and diarrhea are worst during the first 4-6 weeks. As your gut bacteria adapt to the undigested carbs, symptoms usually improve. Studies show that by 6 months, only about 25% of users still report significant flatulence. Patience and slow dose increases make a big difference.
Are alpha-glucosidase inhibitors safe for kidney problems?
Yes. Unlike metformin, which can’t be used in advanced kidney disease, or SGLT2 inhibitors, which require decent kidney function, alpha-glucosidase inhibitors are mostly active in the gut and aren’t cleared by the kidneys. That’s why they’re often chosen for older adults or those with mild to moderate kidney impairment.
What’s the best time to take these drugs?
Take them with the first bite of each main meal. This timing is critical. A 2021 clinical trial showed that taking acarbose with the first bite of food made it 37% more effective than taking it 15 minutes before. The drug needs to be in your intestine at the exact moment carbs arrive to block the enzymes.
Do these drugs work for prediabetes?
Yes. The STOP-NIDDM trial showed that acarbose reduced the chance of developing Type 2 diabetes by 25% in people with prediabetes. Side effects were still common, but because the dose was lower and people were generally healthier, more were able to tolerate them. It’s still used for this purpose in some countries.
Why aren’t these drugs used more often in the U.S.?
Because newer drugs are more effective and easier to tolerate. GLP-1 agonists and SGLT2 inhibitors do more than just lower blood sugar-they protect the heart and kidneys, and help with weight loss. Plus, they don’t cause constant gas. Even though acarbose costs only $15-25 a month, its high discontinuation rate makes it less cost-effective in real-world use.
What Comes Next?
If you’re on an alpha-glucosidase inhibitor and struggling, don’t assume you have to suffer. Talk to your doctor about adjusting your dose, changing your diet, or trying probiotics. If you’ve tried everything and it’s still too much, there are other options-some with fewer side effects, some with added benefits.
If you’re not on one yet but your doctor suggested it, ask: "What’s the plan if the side effects are too much?" Get the dietary advice upfront. Ask for a step-by-step titration schedule. Don’t just take the prescription and hope for the best.
Diabetes management isn’t one-size-fits-all. Sometimes the best tool is the one you can actually live with. For some, that’s an alpha-glucosidase inhibitor. For others, it’s something else. The goal isn’t just to lower numbers-it’s to live well while you do it.
Raja P
December 23, 2025 AT 19:18Man, I’ve been on acarbose for 8 months now and it’s been a game-changer. First month was rough-felt like I was hosting a concert in my gut. But after dialing back the white rice and starting at 25 mg, it got way better. Now I can eat dal-chawal without panic. Also, probiotics helped a ton. Lactobacillus stuff, not the fancy stuff-just plain yogurt daily.
Joseph Manuel
December 23, 2025 AT 22:28The data presented here is statistically sound but lacks clinical context. The 30-50% flatulence rate is well-documented, yet the article fails to address the pharmacoeconomic implications of high discontinuation rates. In a value-based care model, the cost-per-QALY for acarbose is unfavorable compared to GLP-1 RAs, even at $15/month. The tolerability burden outweighs marginal glycemic benefits.
Harsh Khandelwal
December 24, 2025 AT 19:32They don’t want you to know this, but Big Pharma secretly hates acarbose. Why? Because it’s too cheap. They’d rather sell you a $1000/month shot that makes you puke and then charge you extra for the anti-nausea meds. Gas? That’s just your gut saying ‘nope’ to corporate greed. I switched to bitter melon tea and my sugar’s fine. No pills. No gas. No lies.
Andy Grace
December 25, 2025 AT 23:24I’ve seen a few patients on this meds over the years. The key is patience. It’s not that the side effects disappear-they just become background noise. One guy told me after three months, ‘I still fart, but now I just laugh and walk away.’ That’s the real win. And yeah, diet matters more than the pill.
Delilah Rose
December 27, 2025 AT 15:29I think what’s really missing here is the emotional toll of living with constant gastrointestinal discomfort while trying to manage a chronic condition-you’re not just dealing with blood sugar, you’re dealing with shame, social anxiety, the fear of being ‘that person’ at dinner, the awkwardness of excusing yourself after every meal, the way your partner looks at you when you say ‘no, I can’t have bread,’ and then you realize you’ve been avoiding family gatherings for months because you’re too tired of explaining why your gut hates you. It’s not just a side effect-it’s a lifestyle shakedown, and if you’re lucky, you find a rhythm where the benefits outweigh the chaos, but god, it takes time and a lot of self-compassion.
Spencer Garcia
December 28, 2025 AT 03:20Start at 25 mg. Wait two weeks. Eat less white carbs. Use simethicone before meals. No Beano. That’s it. You’ll be fine.
Abby Polhill
December 28, 2025 AT 09:11From a cultural pharmacology standpoint, this is fascinating. In South Asia, where carb-heavy diets are the norm, acarbose is a pragmatic tool-low cost, low systemic risk, and aligned with traditional dietary patterns. Meanwhile, in the U.S., we optimize for convenience and aesthetics, hence the rush to GLP-1s. The drug isn’t obsolete-it’s contextually optimized. Also, the probiotic synergy data is underexplored. L. acidophilus + acarbose = underrated combo.
Bret Freeman
December 29, 2025 AT 17:03THIS IS WHY PEOPLE DIE FROM DIABETES. YOU’RE TELLING SOMEONE TO JUST ‘TOLERATE’ GAS FOR THREE MONTHS? THAT’S NOT MEDICINE, THAT’S TORTURE. MY UNCLE TOOK THIS DRUG AND ENDED UP IN THE ER WITH SEPSIS FROM A BURST DIVERTICULUM BECAUSE HE WAS TOO SCARED TO SAY ‘I CAN’T TAKE THIS ANYMORE.’ DOCTOR’S DON’T LISTEN. THEY JUST HAND OUT PRESCRIPTIONS LIKE CANDY. I’M NOT JUST A PATIENT-I’M A SURVIVOR. AND I WON’T LET THEM DO THIS TO ANYONE ELSE.
Lindsey Kidd
December 29, 2025 AT 20:16Biggest tip: try a low-FODMAP diet for the first month 🌱. It’s not keto, it’s just ‘don’t eat the stuff that makes your colon throw a rave.’ Also, I started with 25 mg and used a little peppermint oil capsule before meals 🌿-so much better than Gas-X. And yes, it gets better! I’m now 6 months in and my sugar’s stable and I can hug my dog without feeling like a balloon. 💪❤️
Austin LeBlanc
December 31, 2025 AT 08:07You’re all missing the point. This drug was designed to make you suffer so you’ll stop eating carbs. That’s the real goal. The ‘blood sugar control’ is just the cover story. If you’re still eating rice and pasta and wondering why you’re bloated, maybe the problem isn’t the drug-it’s your refusal to change. Stop blaming acarbose. Start blaming your cravings.
niharika hardikar
January 1, 2026 AT 04:20While the empirical data on glycemic control is acceptable, the absence of a structured patient education protocol in clinical implementation renders this therapeutic modality suboptimal. The high attrition rate (15–20%) is not a reflection of drug inefficacy but of inadequate pre-prescription counseling. Standardized, multi-session dietary counseling-ideally delivered by certified diabetes care and education specialists-is imperative to improve adherence and mitigate adverse events. Without this, pharmacotherapy remains a blunt instrument.