Dyspepsia Treatment Comparison Tool
Which dyspepsia symptoms do you experience?
Recommended Treatments for Your Symptoms
Acotiamide
Mechanism: Boosts gastric motility by increasing acetylcholine
Best For: Bloating, early satiety, and other motility issues
Onset of Relief: 2-4 weeks
Side Effects: Mild headache, occasional diarrhea
Proton Pump Inhibitors
Mechanism: Reduces stomach acid
Best For: Acid-related pain and reflux
Onset of Relief: 1-2 weeks
Side Effects: Headache, nutrient malabsorption
Key Takeaways
- Acotiamide is the first drug specifically designed to boost stomach motility in functional dyspepsia.
- Clinical trials in Japan and Europe show faster symptom relief than traditional acid‑suppressors.
- Side‑effects are generally mild, with the most common being headache and mild diarrhea.
- It’s approved in Japan and the EU, and is under review by the FDA for U.S. use.
- Patients who do not respond to proton‑pump inhibitors may benefit from a trial of acotiamide.
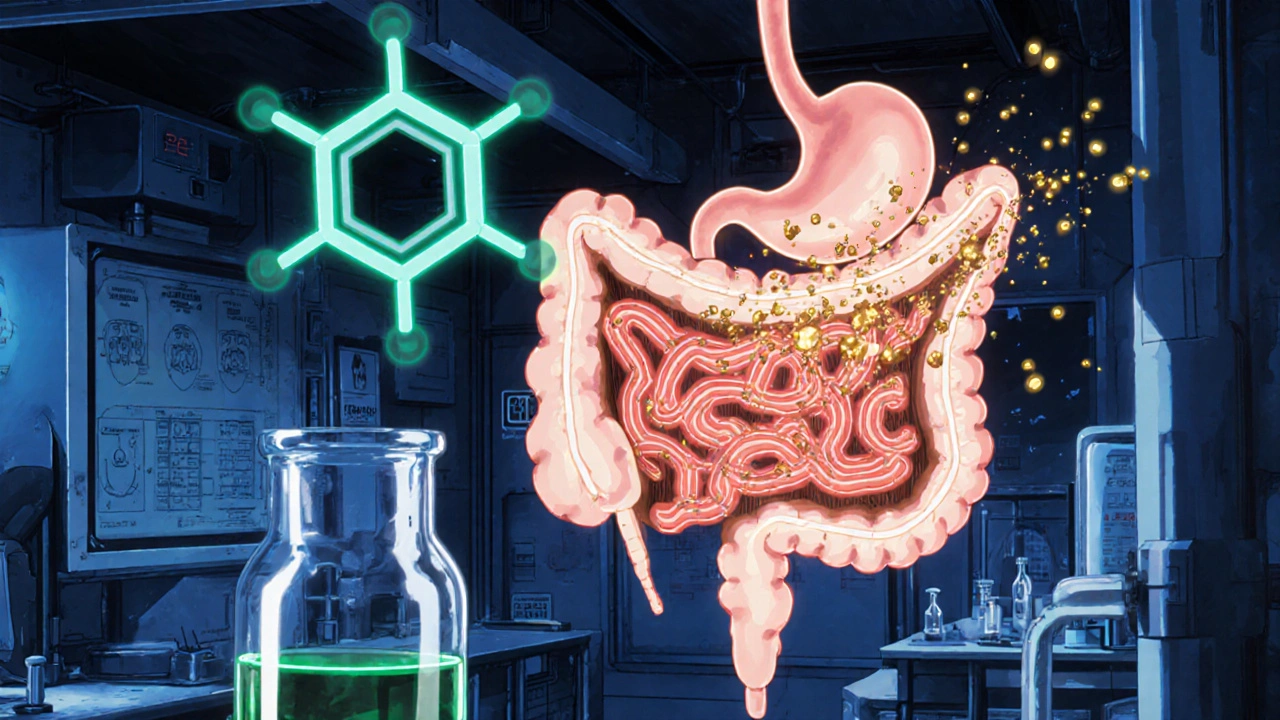
Imagine scrolling through a menu, feeling a knot in your stomach, and then abandoning the meal because the discomfort won’t quit. That’s the everyday reality for millions suffering from dyspepsia. While acid‑suppressing drugs have long been the go‑to solution, they don’t address the underlying motility issue that drives many cases. Enter Acotiamide, a drug that actually helps the stomach move food along. In this guide we’ll break down what acotiamide does, who can benefit, and how it stacks up against older therapies.
What Is Acotiamide?
Acotiamide is a selective acetylcholinesterase inhibitor that enhances acetylcholine activity in the gastrointestinal tract, thereby improving gastric motility. It was first launched in Japan in 2013 under the brand name CAM020 and later received approval in the European Union for the treatment of functional dyspepsia. Unlike proton‑pump inhibitors (PPIs) that reduce stomach acid, acotiamide targets the muscle contractions that push food into the duodenum.
Understanding Dyspepsia and Its Subtypes
Dyspepsia is a broad term covering chronic upper‑abdominal discomfort, early satiety, bloating, and nausea. When investigations (endoscopy, imaging) rule out an ulcer or cancer, the condition is called functional dyspepsia. About 40% of dyspepsia patients fall into this functional category, and the majority experience delayed gastric emptying - a perfect target for a drug that improves stomach muscle activity.
How Acotiamide Works: The Science Simplified
The drug works by inhibiting the breakdown of acetylcholine, a neurotransmitter that tells the stomach’s smooth muscle to contract. Think of acetylcholine as a messenger that says “push!” By keeping more of it around, acotiamide “pushes” food through faster, reducing the sensation of fullness and discomfort. The mechanism can be summed up in this triple:
- Acotiamide inhibits acetylcholinesterase
- Acetylcholinesterase breaks down acetylcholine
- Acetylcholine stimulates gastric motility
Because the drug acts locally in the gut, systemic side‑effects are minimal compared with traditional pro‑kinetic agents like metoclopramide.
Clinical Evidence: What the Trials Show
Two large‑scale, double‑blind, placebo‑controlled trials - the Phase III ACOTIA‑1 and ACOTIA‑2 studies - enrolled a total of 1,571 patients with functional dyspepsia across Japan and Europe. Key findings include:
- After four weeks, 56% of patients on acotiamide reported meaningful symptom relief versus 34% on placebo.
- Gastric emptying time improved by an average of 12 minutes, measured via scintigraphy.
- Adverse events were mild: 8% experienced headache, and 5% reported mild diarrhea.
Follow‑up studies in 2022 confirmed that symptom improvement persists for at least six months with continued dosing, and no serious cardiac or neurological issues were recorded.
Acotiamide vs. Traditional Options
Below is a quick side‑by‑side look at how acotiamide compares with three of the most common dyspepsia treatments.
| Drug | Mechanism | Primary Indication | Onset of Relief | Common Side‑Effects |
|---|---|---|---|---|
| Acotiamide | Acetylcholinesterase inhibition → ↑ acetylcholine → ↑ gastric motility | Functional dyspepsia | 2‑4 weeks | Headache, mild diarrhea |
| Metoclopramide | Dopamine‑D2 receptor antagonist → ↑ GI motility | Gastroparesis, nausea | 1‑2 weeks | Fatigue, extrapyramidal symptoms |
| Proton Pump Inhibitor (e.g., Omeprazole) | H+/K+ ATPase inhibition → ↓ gastric acid | GERD, ulcer‑related dyspepsia | 1‑2 weeks | Headache, nutrient malabsorption |
| H2 Antagonist (e.g., Ranitidine) | Histamine H2 receptor blockade → ↓ acid | Mild acid‑related dyspepsia | 3‑5 days | Confusion, liver enzymes elevation |
Acotiamide’s unique advantage is that it addresses the motility defect directly, which PPIs and H2 antagonists completely ignore. For patients whose main complaint is early satiety and bloating, acotiamide often delivers quicker, more lasting relief.
Who Should Consider Acotiamide?
Ideal candidates are adults diagnosed with functional dyspepsia who have:
- Persistent upper‑abdominal discomfort for at least three months.
- Negative findings on endoscopy (no ulcer or cancer).
- Limited or no improvement with acid‑suppressors.
Patients with severe cardiac disease, recent gastric surgery, or those taking strong CYP3A4 inhibitors should discuss alternatives with their physician, as metabolism interactions are still being studied.
Dosage, Administration, and Safety
The recommended adult dose is 100 mg taken three times daily, 30 minutes before meals. The drug should be swallowed whole; crushing or chewing reduces its efficacy.
- Morning dose - 30 min before breakfast.
- Noon dose - 30 min before lunch.
- Evening dose - 30 min before dinner.
Steady‑state levels are reached after about five days of consistent dosing. If a dose is missed, take it as soon as you remember unless it’s within two hours of the next scheduled dose - then skip the missed one to avoid overdosing.
Safety profile is favorable, but watch for:
- Headache (most common, usually resolves in a week).
- Mild, self‑limiting diarrhea.
- Rare reports of elevated liver enzymes; periodic blood tests are advisable for long‑term users.

Regulatory Status and Availability
Acotiamide holds marketing authorization in Japan (as CAM020) and the European Union (as Foxtan®). The U.S. Food and Drug Administration (FDA) is currently reviewing a New Drug Application (NDA) based on the recent Phase III data. Until approval, U.S. patients can access the medication through qualified online pharmacies that import the drug under a personal use exemption, but they should verify the pharmacy’s licensing.
In Australia, the Therapeutic Goods Administration (TGA) has granted a provisional listing for compassionate use, allowing clinicians to prescribe acotiamide on a case‑by‑case basis.
Practical Tips for Patients
- Keep a symptom diary - note meals, timing of doses, and any side‑effects. This helps your doctor adjust the regimen.
- Avoid heavy, fatty meals during the first two weeks while your gut adjusts.
- Stay hydrated; adequate fluid intake supports gastric motility.
- Combine acotiamide with lifestyle changes (smaller meals, reduced caffeine) for best results.
Frequently Asked Questions
How long does it take for acotiamide to start working?
Most patients notice a reduction in bloating and early satiety within two to four weeks of consistent dosing.
Can I take acotiamide with a proton‑pump inhibitor?
Yes, the two drugs work via different pathways and are often prescribed together when patients have mixed acid‑related and motility symptoms. However, discuss dosing times with your doctor.
Is acotiamide safe for pregnant or breastfeeding women?
Current data are limited; the drug is classified as Category C for pregnancy. Women who are pregnant, planning to become pregnant, or breastfeeding should avoid acotiamide unless the benefits clearly outweigh the risks.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s within two hours of the next scheduled dose. In that case, skip the missed one and continue with your regular schedule.
Are there any drug interactions I should be aware of?
Acotiamide is metabolized primarily by CYP3A4. Strong inhibitors (e.g., ketoconazole) may increase its levels, while inducers (e.g., rifampin) could lower its effectiveness. Always review your medication list with a pharmacist.
Bottom Line
If you’ve been stuck on acid‑suppressors without real relief, acotiamide offers a fresh mechanism that actually helps the stomach move food along. With solid trial data, modest side‑effects, and expanding regulatory approval, it’s quickly becoming the go‑to option for functional dyspepsia. Talk to your gastroenterologist about whether a trial of acotiamide fits your treatment plan.
Shubhi Sahni
October 23, 2025 AT 17:56Thank you for sharing this detailed overview, it’s incredibly helpful, especially for those of us navigating the confusing world of dyspepsia treatments, the way you broke down the mechanism of acotiamide is crystal clear, and the practical tips at the end are a real lifesaver, I encourage anyone reading to keep a symptom diary as suggested, and always consult a gastroenterologist before starting any new regimen.
keerthi yeligay
November 4, 2025 AT 06:43Thx, real clear info!
Simon Waters
November 15, 2025 AT 20:30I can’t help but wonder if the FDA’s review is being influenced by big pharma, the data looks too good to be true, and the speed of approval raises red flags.
CASEY PERRY
November 27, 2025 AT 10:16The pharmacokinetic profile of acotinamide, particularly its CYP3A4-mediated metabolism, warrants rigorous scrutiny in the context of potential drug‑drug interactions, especially given the limited post‑marketing surveillance data.
Danielle St. Marie
December 9, 2025 AT 00:03Honestly, the US has been lagging behind Europe and Japan on this front, we should demand quicker access to such innovative therapies 🇺🇸💪, otherwise we’re just watching the rest of the world move ahead.
Jinny Shin
December 20, 2025 AT 13:50It is truly tragic how many patients suffer in silence while bureaucratic inertia drags their relief further into the abyss.
Mike Peuerböck
January 1, 2026 AT 03:36Acotiamide represents a paradigm shift in the management of functional dyspepsia. By targeting acetylcholinesterase it directly addresses gastric hypomotility rather than merely suppressing acid. The clinical trials disclosed a statistically significant improvement in patient‑reported outcomes compared with placebo. Moreover the safety profile was reassuring with only mild adverse events such as headache and transient diarrhea. Physicians should be aware that the recommended thrice‑daily dosing aligns with meals to maximise its pro‑kinetic effect. Patients who have exhausted proton pump inhibitors may find a meaningful reduction in early satiety after a few weeks of therapy. The mechanism involving acetylcholine preservation also suggests potential synergism when combined with acid‑suppressors. However clinicians must monitor liver enzymes periodically as isolated elevations have been reported. From a pharmacoeconomic perspective the drug may reduce downstream diagnostic testing by alleviating symptom burden early. Real‑world data from Japan indicate improved quality of life scores in the majority of users. Nevertheless the limited availability in the United States remains a barrier for many patients. Health insurers should consider the long‑term cost savings associated with reduced hospital visits. Guidelines are likely to evolve as more evidence accumulates and as regulatory bodies grant formal approval. In the meantime shared decision making remains paramount to tailor therapy to individual tolerance and preference. Overall acotiamide offers a compelling therapeutic option for those struggling with functional dyspepsia where traditional treatments have failed.
Celeste Flynn
January 12, 2026 AT 17:23Clinicians should also educate patients about the importance of lifestyle modifications alongside acotiamide, such as smaller meals and reduced caffeine intake, to optimise outcomes.
Shan Reddy
January 24, 2026 AT 07:10Thanks for the tip, I’ll definitely tell my doc to pair the med with diet changes.
Vikas Kumar
February 4, 2026 AT 20:56Seeing the hype around acotiamide makes me uneasy, it feels like another foreign drug being pushed onto our market without proper scrutiny, and I suspect hidden agendas are at play.